Back
(137) Years of Life Lost from Stimulant-Involved Cardiovascular Mortality, 2014-2023
Saturday, April 26, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2

Rebecca A. Harris, MD, MSc
Assistant Professor of Family Medicine and Community Health
University of Pennsylvania, Pennsylvania
Presenter(s)
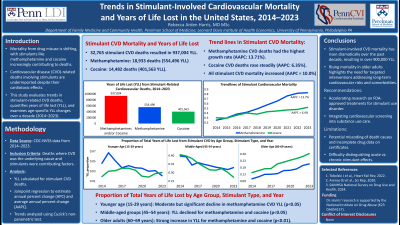
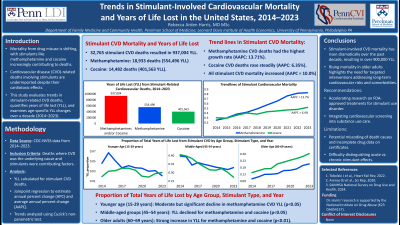
Background & Introduction: Mortality from drug misuse is shifting, with stimulants such as cocaine and methamphetamines contributing to a growing number of deaths. While most reports focus on overdose fatalities, stimulant-related deaths from causes like cardiovascular disease (CVD) are often overlooked, despite the well-documented cardiotoxic effects of these substances. A more comprehensive evaluation of stimulant-related mortality is needed to fully assess their societal impact.
This study focuses on trends in cardiovascular deaths involving stimulants over a 10-year period (2014–2023) among individuals aged 15–69 years. The objectives are to describe trends, quantify total years of life lost (YLL), and analyze age-specific changes in YLL from stimulant-related CVD deaths.
Methods: Using CDC-NVSS data from 2014-2023, we identified all deaths where cardiovascular disease (ICD-10 codes: I00-I99) was the underlying cause and stimulants (methamphetamine: F15, T43.6; cocaine: F14, R78.2, T40.5) were a contributing factor. YLL was calculated for CVD deaths involving methamphetamine, cocaine, or both. Joinpoint regression was used to estimate the annual percent change (APC) and average annual percent change (AAPC) in the rate of stimulant-involved CVD mortality. We also tested for temporal trends in age-specific YLL using Cuzick's non-parametric trends test.
Results: Between 2014 and 2023, there were 32,765 cardiovascular deaths involving cocaine, methamphetamine, or both, resulting in 937,004 YLL in the U.S. Methamphetamines accounted for 18,933 deaths and 554,496 YLL, while cocaine accounted for 14,482 deaths and 401,563 YLL. (The sum of cocaine- and methamphetamine-involved deaths exceeds the total stimulant deaths due to non-duplicative counting of polysubstance cases.)
Joinpoint analysis showed significant increases in stimulant-involved cardiovascular deaths over the past decade. Methamphetamine-related deaths had the highest APCs, with an AAPC of 13.71% (2014–2021: APC 16.66%; 2021–2023: APC 3.98%). Cocaine-involved cardiovascular deaths also rose (AAPC 6.35%) without significant joinpoints. Deaths involving either cocaine, methamphetamine, or both had an AAPC of 10.0%, with a sharp rise from 2014 to 2021 (APC 11.4%) and a slower increase from 2021 to 2023 (APC 5.01%).
Age-group trend analysis showed a moderate but significant decline in methamphetamine-involved CVD YLL for individuals aged 15–29 (p < 0.05). YLL for middle-aged groups (45–54 years) declined across all stimulants (p < 0.05). In contrast, adults aged 60–69 had a strong, significant increase in YLL for methamphetamine, cocaine, and all stimulants combined (p < 0.01).
Conclusion & Discussion: Stimulant-involved cardiovascular mortality has sharply increased over the past decade, leading to more than 900,000 years of life lost. Age-specific analysis showed declining mortality in middle-aged adults (45–54 years), possibly due to changing drug use patterns, harm reduction efforts, and better treatment access. In contrast, older adults (60–69 years) had rising death rates, likely due to long-term cardiovascular damage, increased heart disease risk, and growing stimulant use in this group. Comorbidities and polydrug use further heighten cardiovascular risks in older individuals.
The lack of FDA-approved treatments for stimulant use disorder underscores the need for accelerated pharmacological research and evidence-based training for addiction specialists, primary care providers, and cardiologists. Integrating cardiovascular screening into substance use care could reduce stimulant-related deaths. Study limitations include potential miscoding of causes of death, incomplete drug data on death certificates, and difficulties distinguishing acute from chronic stimulant effects.
References: 1. Tobolski J, Sawyer DB, Song SJ, Afari ME. Cardiovascular disease associated with methamphetamine use: a review. Heart Fail Rev. 2022;27(6):2059-2065. doi:10.1007/s10741-022-10261-7
2. Phillips K, Luk A, Soor GS, Abraham JR, Leong S, Butany J. Cocaine cardiotoxicity: a review of the pathophysiology, pathology, and treatment options. Am J Cardiovasc Drugs. 2009;9(3):177-196. doi:10.2165/00129784-200909030-00005
3. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2023 National Survey on Drug Use and Health. HHS Publication No. PEP24-07-021, NSDUH Series H-59. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2024. https://www.samhsa.gov/data/report/2023-nsduh-annual-national-report
4. Centers for Disease Control and Prevention, National Center for Health Statistics. National
Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. Data are
from the final Multiple Cause of Death Files, 2018-2022, and from provisional data for year
2023, as compiled from data provided by the 57 vital statistics jurisdictions through the
Vital Statistics Cooperative Program. Accessed at https://wonder.cdc.gov/mcd-icd10-
provisional.html. Accessed October 8, 2024.
5. Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential - United States, 2003-2017. MMWR Morb Mortal Wkly Rep. 2019;68(17):388-395. Published 2019 May 3. doi:10.15585/mmwr.mm6817a3
This study focuses on trends in cardiovascular deaths involving stimulants over a 10-year period (2014–2023) among individuals aged 15–69 years. The objectives are to describe trends, quantify total years of life lost (YLL), and analyze age-specific changes in YLL from stimulant-related CVD deaths.
Methods: Using CDC-NVSS data from 2014-2023, we identified all deaths where cardiovascular disease (ICD-10 codes: I00-I99) was the underlying cause and stimulants (methamphetamine: F15, T43.6; cocaine: F14, R78.2, T40.5) were a contributing factor. YLL was calculated for CVD deaths involving methamphetamine, cocaine, or both. Joinpoint regression was used to estimate the annual percent change (APC) and average annual percent change (AAPC) in the rate of stimulant-involved CVD mortality. We also tested for temporal trends in age-specific YLL using Cuzick's non-parametric trends test.
Results: Between 2014 and 2023, there were 32,765 cardiovascular deaths involving cocaine, methamphetamine, or both, resulting in 937,004 YLL in the U.S. Methamphetamines accounted for 18,933 deaths and 554,496 YLL, while cocaine accounted for 14,482 deaths and 401,563 YLL. (The sum of cocaine- and methamphetamine-involved deaths exceeds the total stimulant deaths due to non-duplicative counting of polysubstance cases.)
Joinpoint analysis showed significant increases in stimulant-involved cardiovascular deaths over the past decade. Methamphetamine-related deaths had the highest APCs, with an AAPC of 13.71% (2014–2021: APC 16.66%; 2021–2023: APC 3.98%). Cocaine-involved cardiovascular deaths also rose (AAPC 6.35%) without significant joinpoints. Deaths involving either cocaine, methamphetamine, or both had an AAPC of 10.0%, with a sharp rise from 2014 to 2021 (APC 11.4%) and a slower increase from 2021 to 2023 (APC 5.01%).
Age-group trend analysis showed a moderate but significant decline in methamphetamine-involved CVD YLL for individuals aged 15–29 (p < 0.05). YLL for middle-aged groups (45–54 years) declined across all stimulants (p < 0.05). In contrast, adults aged 60–69 had a strong, significant increase in YLL for methamphetamine, cocaine, and all stimulants combined (p < 0.01).
Conclusion & Discussion: Stimulant-involved cardiovascular mortality has sharply increased over the past decade, leading to more than 900,000 years of life lost. Age-specific analysis showed declining mortality in middle-aged adults (45–54 years), possibly due to changing drug use patterns, harm reduction efforts, and better treatment access. In contrast, older adults (60–69 years) had rising death rates, likely due to long-term cardiovascular damage, increased heart disease risk, and growing stimulant use in this group. Comorbidities and polydrug use further heighten cardiovascular risks in older individuals.
The lack of FDA-approved treatments for stimulant use disorder underscores the need for accelerated pharmacological research and evidence-based training for addiction specialists, primary care providers, and cardiologists. Integrating cardiovascular screening into substance use care could reduce stimulant-related deaths. Study limitations include potential miscoding of causes of death, incomplete drug data on death certificates, and difficulties distinguishing acute from chronic stimulant effects.
References: 1. Tobolski J, Sawyer DB, Song SJ, Afari ME. Cardiovascular disease associated with methamphetamine use: a review. Heart Fail Rev. 2022;27(6):2059-2065. doi:10.1007/s10741-022-10261-7
2. Phillips K, Luk A, Soor GS, Abraham JR, Leong S, Butany J. Cocaine cardiotoxicity: a review of the pathophysiology, pathology, and treatment options. Am J Cardiovasc Drugs. 2009;9(3):177-196. doi:10.2165/00129784-200909030-00005
3. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2023 National Survey on Drug Use and Health. HHS Publication No. PEP24-07-021, NSDUH Series H-59. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2024. https://www.samhsa.gov/data/report/2023-nsduh-annual-national-report
4. Centers for Disease Control and Prevention, National Center for Health Statistics. National
Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. Data are
from the final Multiple Cause of Death Files, 2018-2022, and from provisional data for year
2023, as compiled from data provided by the 57 vital statistics jurisdictions through the
Vital Statistics Cooperative Program. Accessed at https://wonder.cdc.gov/mcd-icd10-
provisional.html. Accessed October 8, 2024.
5. Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential - United States, 2003-2017. MMWR Morb Mortal Wkly Rep. 2019;68(17):388-395. Published 2019 May 3. doi:10.15585/mmwr.mm6817a3
Learning Objectives:
- Analyze trends in stimulant-involved cardiovascular mortality from 2014-2023, comparing the impact of methamphetamine and cocaine on years of life lost in the U.S.
- Differentiate age-specific changes in years of life lost from stimulant-related cardiovascular deaths, with a focus on divergent trends among young, middle-aged, and older adults.
- Evaluate the need for integrated cardiovascular screening and novel treatments for stimulant use disorder in light of rising cardiovascular mortality, particularly among older adults.
