Back
(57) Impact of Gabapentin Regulation on Opioid Overdose Trends, 2013-2022
Friday, April 25, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2

Conrad Say, Medical Student
Medical Student
Baylor College of Medicine, Texas- HF
Hiroko Furo, MD, PhD
Associate Professor
Baylor College of Medicine, Texas
Presenter(s)
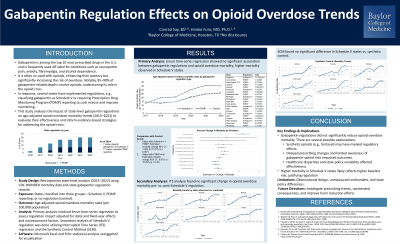
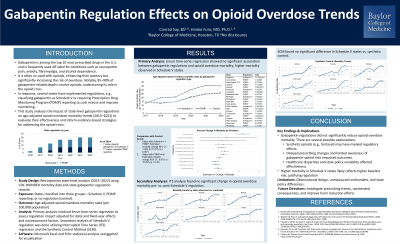
Background & Introduction: Gabapentin, one of the top 10 most prescribed medications in the U.S., is widely used off-label for indications such as neuropathic pain, anxiety, fibromyalgia, and alcohol dependence. While gabapentin offers therapeutic benefits, its misuse has become a growing concern. Gabapentin is frequently co-used with opioids, as it enhances opioid potency, increasing the risk of overdose with respiratory depression. Studies report that opioids are detected in 85–90% of gabapentin-related deaths, highlighting its potential role in the recent opioid crisis in the U.S.
To address these concerns, several states have implemented regulations for gabapentin, including classifying it as a Schedule V controlled substance and/or requiring its monitoring through Prescription Drug Monitoring Programs (PDMPs). These measures aim to improve monitoring and reduce misuse. However, the effectiveness of such regulations in mitigating opioid overdose deaths remains unclear and under explored.
This study evaluates the impact of state-level gabapentin regulations on age-adjusted opioid overdose mortality trends in the U.S. from 2013 to 2022. By analyzing data from states with varying regulatory approaches, this research aims to assess the effectiveness of these policies and provide valuable insights into strategies for addressing the current opioid crisis in the U.S.
Methods: The current regulation on gabapentin in each state was reviewed using official state websites. Age-adjusted opioid overdose mortality data from 2013 to 2022 were obtained from the Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) database, using the following two groups of ICD-10 codes: 1) substance related mortality (T39, T40.5, 7-9, T42, 3-7, T43.6-7, T43.6, 8-9, T51.0, X40-45, X60-65, Y10-15), and 2) opioid related mortality (T39, 40.0-4, 6).
A linear time-series regression model was used to look for an association between gabapentin regulations and opioid-related overdose mortality. We used following variables to analyze the data: state and year fixed effects and socioeconomic factors, including annual state unemployment rates, poverty rates, and the percentage of the population with a bachelor’s degree.
Secondary analyses were conducted utilizing an interrupted time-series (ITS) regression to explore the rate of rise (ROR) of opioid-related overdose mortality before and after state regulation. Additionally, the synthetic control method (SCM) was applied to generate comparison groups, to further validate the findings. These approaches provided a comprehensive assessment of the impact of gabapentin regulation on opioid overdose mortality rates at intra-state and interstate levels.
Results: State regulations on gabapentin controlled substance status were reviewed. We found that 7 states have classified gabapentin as a Schedule V controlled substance and 17 states have required PDMP reporting. The 7 Schedule V controlled substance states and their enactment dates are listed as follows: Alabama (11/18/2019), Kentucky (07/01/2017), Michigan (01/04/2019, which was repealed in 2024), North Dakota (08/01/2020), Tennessee (07/01/2018), Virginia (07/01/2019), and West Virginia (06/05/2018). The 17 PDMP states are: Connecticut (01/01/2021), District of Columbia (06/07/2019), Indiana (07/01/2019), Kansas (07/25/2018), Louisiana (01/20/2021), Massachusetts (08/01/2017), Minnesota (08/01/2016), Nebraska (01/01/2018), New Jersey (05/07/2018), North Carolina (03/01/2024), North Dakota (08/01/2019 *Note difference in years), Ohio (12/01/2016), Oregon (01/01/2020), Utah (12/09/2019), Virginia (02/23/2017 *Note difference in years), Wisconsin (09/01/2021), and Wyoming (07/01/2017). Then these states are categorized into 3 groups: 1) Scheduled V controlled substance states, 2) PDMP only states and 3) the rest (control states). The association between this variable and overall opioid overdose mortality rates were analyzed. Our analysis showed no statistically significant differences in overall opioid overdose mortality rates between regulated and non-regulated states. States with Schedule V classification and PDMP reporting demonstrated an estimated change in mortality rates of 95% CI, -1.58% to 27.27% (p = 0.087), while states with PDMP-only regulation showed a change of 95% CI, -6.07% to 15.29% (p = 0.45). These results indicate that neither type of regulation had a measurable impact on reducing opioid overdose mortality across the study population.
Secondary analyses, including interrupted time-series (ITS) regression, further validated these findings. No significant changes in the rate of rise (ROR) of opioid overdose mortality were observed in regulated states following the implementation of gabapentin regulations. Similarly, the synthetic control method (SCM) confirmed the lack of consistent differences among the three state groups when comparing pre- and post-regulation trends.
Despite the overall lack of significant results, some states showed modest reductions in opioid overdose mortality trends after implementing regulations. These localized improvements suggest that other factors, such as robust PDMP utilization, targeted public health initiatives, or clinician education, may enhance the effectiveness of gabapentin regulation. For example, states with comprehensive PDMP systems or active community engagement programs observed minor declines in opioid overdose deaths, although these trends were not statistically significant at the aggregate level.
Conclusion & Discussion: Our study found that state-level gabapentin regulations did not significantly reduce overall opioid overdose mortality rates between 2013 and 2022. However, some states demonstrated modest improvements in overdose death rates following regulatory implementation, suggesting potential localized benefits. These findings highlight the complexity of addressing opioid-related mortality through the regulation of a single medication and underscore the multifactorial nature of the opioid crisis.
Several factors may explain the limited overall impact of gabapentin regulations. Variations in how states implement and enforce regulations likely contribute to differences in effectiveness. Furthermore, disparities in healthcare infrastructure, the availability of harm-reduction resources like naloxone and addiction treatment services, and clinician education may play crucial roles. Socioeconomic and demographic factors, such as poverty, education, and cultural attitudes toward substance use, could also influence outcomes.
Future research should investigate intra-state factors that contribute to reductions in mortality in certain states. Enhanced PDMP utilization, public health campaigns, and tailored policy approaches may explain localized improvements. Additionally, examining unintended consequences, such as reduced access to gabapentin for legitimate medical purposes, is critical.
References: 1. Kuehn BM. Growing Role of Gabapentin in Opioid-Related Overdoses Highlights Misuse Potential and Off-label Prescribing Practices. JAMA. 2022;328(13):1283–1285. doi:10.1001/jama.2022.13659
2. Wallach JD, Ross JS. Gabapentin Approvals, Off-Label Use, and Lessons for Postmarketing Evaluation Efforts. JAMA. 2018;319(8):776–778. doi:10.1001/jama.2017.21897
3. Fukada C, Kohler JC, Boon H, Austin Z, Krahn M. Prescribing gabapentin off label: Perspectives from psychiatry, pain and neurology specialists. Can Pharm J (Ott). 2012 Nov;145(6):280-284.e1. doi: 10.3821/145.6.cpj280. PMID: 23509590; PMCID: PMC3567599.
4. Karavolis ZA, Su AB, Peckham AM. State-level response to gabapentin misuse in the United States: Implications and future direction. Am J Health-Syst Pharm. 2022 May 1;79(9):e143–e148. doi: 10.1093/ajhp/zxab486.
5. Centers for Disease Control and Prevention (CDC). WONDER platform. Accessed January 8, 2025. https://wonder.cdc.gov/
To address these concerns, several states have implemented regulations for gabapentin, including classifying it as a Schedule V controlled substance and/or requiring its monitoring through Prescription Drug Monitoring Programs (PDMPs). These measures aim to improve monitoring and reduce misuse. However, the effectiveness of such regulations in mitigating opioid overdose deaths remains unclear and under explored.
This study evaluates the impact of state-level gabapentin regulations on age-adjusted opioid overdose mortality trends in the U.S. from 2013 to 2022. By analyzing data from states with varying regulatory approaches, this research aims to assess the effectiveness of these policies and provide valuable insights into strategies for addressing the current opioid crisis in the U.S.
Methods: The current regulation on gabapentin in each state was reviewed using official state websites. Age-adjusted opioid overdose mortality data from 2013 to 2022 were obtained from the Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) database, using the following two groups of ICD-10 codes: 1) substance related mortality (T39, T40.5, 7-9, T42, 3-7, T43.6-7, T43.6, 8-9, T51.0, X40-45, X60-65, Y10-15), and 2) opioid related mortality (T39, 40.0-4, 6).
A linear time-series regression model was used to look for an association between gabapentin regulations and opioid-related overdose mortality. We used following variables to analyze the data: state and year fixed effects and socioeconomic factors, including annual state unemployment rates, poverty rates, and the percentage of the population with a bachelor’s degree.
Secondary analyses were conducted utilizing an interrupted time-series (ITS) regression to explore the rate of rise (ROR) of opioid-related overdose mortality before and after state regulation. Additionally, the synthetic control method (SCM) was applied to generate comparison groups, to further validate the findings. These approaches provided a comprehensive assessment of the impact of gabapentin regulation on opioid overdose mortality rates at intra-state and interstate levels.
Results: State regulations on gabapentin controlled substance status were reviewed. We found that 7 states have classified gabapentin as a Schedule V controlled substance and 17 states have required PDMP reporting. The 7 Schedule V controlled substance states and their enactment dates are listed as follows: Alabama (11/18/2019), Kentucky (07/01/2017), Michigan (01/04/2019, which was repealed in 2024), North Dakota (08/01/2020), Tennessee (07/01/2018), Virginia (07/01/2019), and West Virginia (06/05/2018). The 17 PDMP states are: Connecticut (01/01/2021), District of Columbia (06/07/2019), Indiana (07/01/2019), Kansas (07/25/2018), Louisiana (01/20/2021), Massachusetts (08/01/2017), Minnesota (08/01/2016), Nebraska (01/01/2018), New Jersey (05/07/2018), North Carolina (03/01/2024), North Dakota (08/01/2019 *Note difference in years), Ohio (12/01/2016), Oregon (01/01/2020), Utah (12/09/2019), Virginia (02/23/2017 *Note difference in years), Wisconsin (09/01/2021), and Wyoming (07/01/2017). Then these states are categorized into 3 groups: 1) Scheduled V controlled substance states, 2) PDMP only states and 3) the rest (control states). The association between this variable and overall opioid overdose mortality rates were analyzed. Our analysis showed no statistically significant differences in overall opioid overdose mortality rates between regulated and non-regulated states. States with Schedule V classification and PDMP reporting demonstrated an estimated change in mortality rates of 95% CI, -1.58% to 27.27% (p = 0.087), while states with PDMP-only regulation showed a change of 95% CI, -6.07% to 15.29% (p = 0.45). These results indicate that neither type of regulation had a measurable impact on reducing opioid overdose mortality across the study population.
Secondary analyses, including interrupted time-series (ITS) regression, further validated these findings. No significant changes in the rate of rise (ROR) of opioid overdose mortality were observed in regulated states following the implementation of gabapentin regulations. Similarly, the synthetic control method (SCM) confirmed the lack of consistent differences among the three state groups when comparing pre- and post-regulation trends.
Despite the overall lack of significant results, some states showed modest reductions in opioid overdose mortality trends after implementing regulations. These localized improvements suggest that other factors, such as robust PDMP utilization, targeted public health initiatives, or clinician education, may enhance the effectiveness of gabapentin regulation. For example, states with comprehensive PDMP systems or active community engagement programs observed minor declines in opioid overdose deaths, although these trends were not statistically significant at the aggregate level.
Conclusion & Discussion: Our study found that state-level gabapentin regulations did not significantly reduce overall opioid overdose mortality rates between 2013 and 2022. However, some states demonstrated modest improvements in overdose death rates following regulatory implementation, suggesting potential localized benefits. These findings highlight the complexity of addressing opioid-related mortality through the regulation of a single medication and underscore the multifactorial nature of the opioid crisis.
Several factors may explain the limited overall impact of gabapentin regulations. Variations in how states implement and enforce regulations likely contribute to differences in effectiveness. Furthermore, disparities in healthcare infrastructure, the availability of harm-reduction resources like naloxone and addiction treatment services, and clinician education may play crucial roles. Socioeconomic and demographic factors, such as poverty, education, and cultural attitudes toward substance use, could also influence outcomes.
Future research should investigate intra-state factors that contribute to reductions in mortality in certain states. Enhanced PDMP utilization, public health campaigns, and tailored policy approaches may explain localized improvements. Additionally, examining unintended consequences, such as reduced access to gabapentin for legitimate medical purposes, is critical.
References: 1. Kuehn BM. Growing Role of Gabapentin in Opioid-Related Overdoses Highlights Misuse Potential and Off-label Prescribing Practices. JAMA. 2022;328(13):1283–1285. doi:10.1001/jama.2022.13659
2. Wallach JD, Ross JS. Gabapentin Approvals, Off-Label Use, and Lessons for Postmarketing Evaluation Efforts. JAMA. 2018;319(8):776–778. doi:10.1001/jama.2017.21897
3. Fukada C, Kohler JC, Boon H, Austin Z, Krahn M. Prescribing gabapentin off label: Perspectives from psychiatry, pain and neurology specialists. Can Pharm J (Ott). 2012 Nov;145(6):280-284.e1. doi: 10.3821/145.6.cpj280. PMID: 23509590; PMCID: PMC3567599.
4. Karavolis ZA, Su AB, Peckham AM. State-level response to gabapentin misuse in the United States: Implications and future direction. Am J Health-Syst Pharm. 2022 May 1;79(9):e143–e148. doi: 10.1093/ajhp/zxab486.
5. Centers for Disease Control and Prevention (CDC). WONDER platform. Accessed January 8, 2025. https://wonder.cdc.gov/
Learning Objectives:
- evaluate the methodologies used to assess the impact of gabapentin regulations on opioid overdose mortality trends, including time-series regression and synthetic control methods.
- Describe the key factors, such as state-level regulatory approaches, healthcare infrastructure, and socioeconomic influences, that affect the efficacy of gabapentin regulations in reducing opioid-related mortality.
- Discuss potential strategies, including enhanced PDMP utilization, clinician education, and public health initiatives, to improve the effectiveness of gabapentin regulations and address opioid-related harms.
