Back
(127) Initiating Extended-Release Injectable Buprenorphine in Primary Care without a Test Dose
Saturday, April 26, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2

Linda Wang, MD
Assistant Professor of Medicine & Medical Education
Icahn School of Medicine at Mount Sinai, New York- ES
Emily Scognamiglio, MPH
Registered Nurse
Icahn School of Medicine, New York
Presenter(s)
Non-presenting author(s)
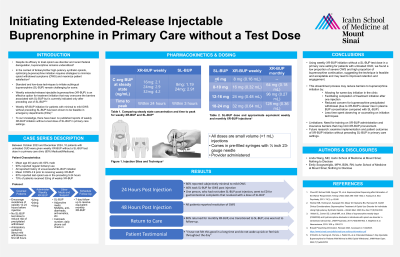
Background & Introduction: Despite its efficacy to treat opioid use disorder (OUD) and recent federal deregulation, buprenorphine remains underutilized (1). In the context of fentanyl and other high-potency synthetic opioids, optimizing buprenorphine initiation requires strategies to minimize opioid withdrawal symptoms (OWS) and maximize patient satisfaction (2). Current approaches to initiate sublingual buprenorphine (SL-BUP) remain challenging: standard techniques require patients to experience moderate OWS before starting and low-dose techniques advise patients to continue a concurrent full agonist opioid, either of which may be unacceptable to patients. Providers may find these techniques logistically complicated, especially in busy primary care settings where it is difficult to observe patients or provide lengthy counseling. Weekly extended-release injectable buprenorphine (XR-BUP) is an effective option for treatment initiation that may overcome the barriers associated with SL-BUP but is currently indicated only after a test dose of SL-BUP (3, 4). Weekly XR-BUP initiation for patients with minimal to mild OWS without preceding SL-BUP has been shown to be feasible in emergency departments (EDs) (5). To our knowledge, there have been no published reports of weekly XR-BUP initiation without a test dose of SL-BUP in primary care settings.
Case Description: This case series describes the protocol and reviews the initial outcomes of 10 cases of weekly XR-BUP initiation without a SL-BUP test dose for patients with untreated OUD in a primary care clinic between October 2023 and December 2024. More than 80% of the clinic’s patient population are Medicaid/Medicare beneficiaries. The protocol is informed by the approach used in the aforementioned ED study of weekly XR-BUP initiation and our own clinical experiences.
All patients were provided information about SL-BUP and weekly XR-BUP initiation approaches and agreed to XR-BUP initiation. In all cases, patients reported regularly using non-prescribed opioids, and all but 1 reported using fentanyl. All patients reported a history of unsuccessful SL-BUP initiation. All patients were encouraged to not use opioids for 12-24 hours prior to their scheduled appointment. Since they were expected to have minimal to mild OWS at time of injection (COWS < 8), patients were counseled to not take any previously prescribed SL-BUP to reduce the risk of precipitated withdrawal. Patients were given a weekly XR-BUP injection (16mg, 24mg, or 32mg) and prescribed SL-BUP to use for any additional OWS or cravings experienced during the week after injection. Patients were scheduled for a 7-day clinic follow-up to receive their monthly XR-BUP injection. No patients were observed in the clinic for symptom management after injection.
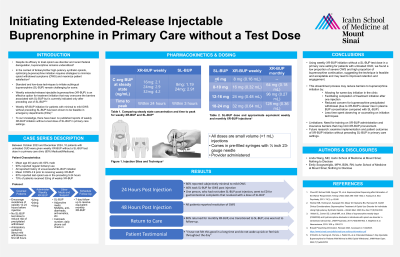
Most patients were male (60%) and the mean age was 46 years old. The mean COWS prior to receiving the weekly XR-BUP was 4.9 (standard deviation 5.2). For most patients (80%), reported last opioid use was in the preceding 5-24 hours. Most patients received 32mg of weekly XR-BUP (70%). At 24 hours post-injection, most patients reported subjectively minimal to mild OWS (80%) and less than half took SL-BUP for OWS (40%); one patient who had not taken SL-BUP went to the ED for gastrointestinal complaints, which resolved with a dose of SL-BUP. All patients reported resolution of OWS by 48 hours post-injection. Most patients (80%) returned for a monthly XR-BUP injection, one patient transitioned to SL-BUP instead of monthly XR-BUP and one patient was lost to follow-up. One patient reported they “had not felt this good in a long time,” and that they no longer woke up with OWS or felt OWS throughout the day after their weekly XR-BUP injection.
Conclusion & Discussion: We describe a novel approach using weekly XR-BUP initiation without a SL-BUP test dose in a primary care setting for patients with untreated OUD. The low proportion of severe OWS and high proportion of buprenorphine treatment continuation suggest the technique is feasible and acceptable. Almost all patients experienced mild OWS that resolved by 48 hours and was managed with or without SL-BUP. This outcome, likely due to XR-BUP’s slower rise in plasma buprenorphine concentration compared with sublingual, may encourage patients who are concerned about buprenorphine precipitated withdrawal, which is reported as a barrier to SL-BUP uptake. For providers, this protocol created a streamlined process which may reduce logistical challenges, including the option for buprenorphine initiation the same-day as presentation, minimal concern for significant adverse effects and less time spent observing patients or counseling on complicated initiation techniques. Importantly, because 90% of patients returned for treatment continuation, weekly XR-BUP initiation may lead to improved retention and engagement, which have been demonstrated to reduce overdose risk. Limitations include the need for training on XR-BUP administration and insurance barriers that may limit XR-BUP procurement. Future research should examine the implementation and patient outcomes of XR-BUP initiation without preceding SL-BUP in primary care settings.
References: 1. Chua KP, Bohnert ASB, Nyugen TD, et al. Buprenorphine Dispensing after Elimination of the Waiver Requirement. N Engl J Med 2024;390:1530-1532
2. Weimer MB, Herring AA, Kawasaki SS, Meyer M, Kleykamp BA, Ramsey KS. ASAM Clinical Considerations: Buprenorphine Treatment of Opioid Use Disorder for Individuals Using High-potency Synthetic Opioids. J Addict Med. 2023 Nov-Dec;17(6):632-639
3. Walsh SL, Comer SD, Lofwall MR, et al. Effect of buprenorphine weekly depot (CAM2038) and hydromorphone blockade in individuals with opioid use disorder: a randomized clinical trial. JAMA Psychiatry. 2017;74(9):894-902.
4. Brixadi Prescribing Information. Revised 2023. Accessed on 1/22/2025. https://www.brixadi.com/pdfs/brixadi-prescribing-information.pdf
5. D’Onofrio G, Herring AA, Perrone J, Fiellin DA, et al. Extended-Release 7-Day Injectable Buprenorphine for Patients With Minimal to Mild Opioid Withdrawal. JAMA Netw Open. 2024;7(7):e2420702
Case Description: This case series describes the protocol and reviews the initial outcomes of 10 cases of weekly XR-BUP initiation without a SL-BUP test dose for patients with untreated OUD in a primary care clinic between October 2023 and December 2024. More than 80% of the clinic’s patient population are Medicaid/Medicare beneficiaries. The protocol is informed by the approach used in the aforementioned ED study of weekly XR-BUP initiation and our own clinical experiences.
All patients were provided information about SL-BUP and weekly XR-BUP initiation approaches and agreed to XR-BUP initiation. In all cases, patients reported regularly using non-prescribed opioids, and all but 1 reported using fentanyl. All patients reported a history of unsuccessful SL-BUP initiation. All patients were encouraged to not use opioids for 12-24 hours prior to their scheduled appointment. Since they were expected to have minimal to mild OWS at time of injection (COWS < 8), patients were counseled to not take any previously prescribed SL-BUP to reduce the risk of precipitated withdrawal. Patients were given a weekly XR-BUP injection (16mg, 24mg, or 32mg) and prescribed SL-BUP to use for any additional OWS or cravings experienced during the week after injection. Patients were scheduled for a 7-day clinic follow-up to receive their monthly XR-BUP injection. No patients were observed in the clinic for symptom management after injection.
Most patients were male (60%) and the mean age was 46 years old. The mean COWS prior to receiving the weekly XR-BUP was 4.9 (standard deviation 5.2). For most patients (80%), reported last opioid use was in the preceding 5-24 hours. Most patients received 32mg of weekly XR-BUP (70%). At 24 hours post-injection, most patients reported subjectively minimal to mild OWS (80%) and less than half took SL-BUP for OWS (40%); one patient who had not taken SL-BUP went to the ED for gastrointestinal complaints, which resolved with a dose of SL-BUP. All patients reported resolution of OWS by 48 hours post-injection. Most patients (80%) returned for a monthly XR-BUP injection, one patient transitioned to SL-BUP instead of monthly XR-BUP and one patient was lost to follow-up. One patient reported they “had not felt this good in a long time,” and that they no longer woke up with OWS or felt OWS throughout the day after their weekly XR-BUP injection.
Conclusion & Discussion: We describe a novel approach using weekly XR-BUP initiation without a SL-BUP test dose in a primary care setting for patients with untreated OUD. The low proportion of severe OWS and high proportion of buprenorphine treatment continuation suggest the technique is feasible and acceptable. Almost all patients experienced mild OWS that resolved by 48 hours and was managed with or without SL-BUP. This outcome, likely due to XR-BUP’s slower rise in plasma buprenorphine concentration compared with sublingual, may encourage patients who are concerned about buprenorphine precipitated withdrawal, which is reported as a barrier to SL-BUP uptake. For providers, this protocol created a streamlined process which may reduce logistical challenges, including the option for buprenorphine initiation the same-day as presentation, minimal concern for significant adverse effects and less time spent observing patients or counseling on complicated initiation techniques. Importantly, because 90% of patients returned for treatment continuation, weekly XR-BUP initiation may lead to improved retention and engagement, which have been demonstrated to reduce overdose risk. Limitations include the need for training on XR-BUP administration and insurance barriers that may limit XR-BUP procurement. Future research should examine the implementation and patient outcomes of XR-BUP initiation without preceding SL-BUP in primary care settings.
References: 1. Chua KP, Bohnert ASB, Nyugen TD, et al. Buprenorphine Dispensing after Elimination of the Waiver Requirement. N Engl J Med 2024;390:1530-1532
2. Weimer MB, Herring AA, Kawasaki SS, Meyer M, Kleykamp BA, Ramsey KS. ASAM Clinical Considerations: Buprenorphine Treatment of Opioid Use Disorder for Individuals Using High-potency Synthetic Opioids. J Addict Med. 2023 Nov-Dec;17(6):632-639
3. Walsh SL, Comer SD, Lofwall MR, et al. Effect of buprenorphine weekly depot (CAM2038) and hydromorphone blockade in individuals with opioid use disorder: a randomized clinical trial. JAMA Psychiatry. 2017;74(9):894-902.
4. Brixadi Prescribing Information. Revised 2023. Accessed on 1/22/2025. https://www.brixadi.com/pdfs/brixadi-prescribing-information.pdf
5. D’Onofrio G, Herring AA, Perrone J, Fiellin DA, et al. Extended-Release 7-Day Injectable Buprenorphine for Patients With Minimal to Mild Opioid Withdrawal. JAMA Netw Open. 2024;7(7):e2420702
Learning Objectives:
- Describe a patient-level barrier to initiating sublingual buprenorphine.
- Describe the current indication for extended-release injectable buprenorphine.
- Report one patient-related outcome related to extended-release injectable buprenorphine initiation without preceding sublingual dose
