Back
(75) Optimizing Telephone Call Reminders to Improve Appointment Attendance at Outpatient Clinic
Saturday, April 26, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2
- BO
Bridget Oppong-Darko, DNP, FNP-C, RN
Clinical Associate Professor
Binghamton University - Decker College of Nursing and Health Sciences, New York
Presenter(s)
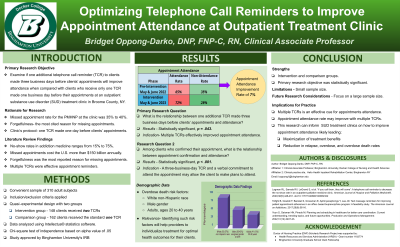
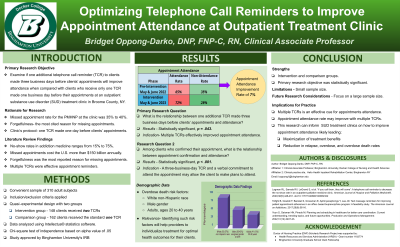
Background & Introduction: Millions of Americans are affected by substance use disorder (SUD). Appointment no-show rates in addiction medicine range from 15 to 75% for both initial and follow-up appointments (3). Treating individuals with SUD often presents a unique set of challenges, which can be made even more complex when patients miss their scheduled appointments. Such challenges include poor health outcomes, treatment non-adherence, relapse, and increased premature mortality rates (4). Missed appointments directly cost the United States healthcare system more than $150 billion annually, and individual providers lose about $200 for every unused appointment time slot (5). Individuals who remain in treatment for an extended period achieve decreased relapse rates and overdose prevention. Hence, practical strategies are needed to engage and maintain patients in treatment. The most cited reason for missing outpatient appointments is forgetfulness and implementing telephone call reminders (TCRs) showed a decrease in missed appointments (1). The primary objective of this study was to examine if one additional TCR to clients made three business days before their scheduled appointments will improve appointment attendance when compared with clients who receive only one TCR made one business day before their appointments. Other outcome variables were analyzed.
Methods: This eight-week-long study used a quasi‐experimental design with intervention and comparison groups at an outpatient SUD treatment clinic in Broome County, New York. The intervention group received the three-business day TCR in addition to the clinic's standard protocol of one TCR to clients one business day before their scheduled appointments. The comparison group received the clinic’s standard protocol of one TCR. The primary research question: What is the relationship between one additional TCR three business days before clients’ appointments and attendance? Question 2: What is the relationship between appointment confirmation and attendance? Question 3: What is the relationship between SUD diagnosis type and appointment attendance? Question 4: What is the relationship between the SUD diagnosis severity level and appointment attendance? A convenient sample of 338 adult subjects were enrolled. After inclusion and exclusion criteria were applied, 310 subjects remained with 148 and 162 in the intervention and comparison groups, respectively. Appointment attendance was the dependent variable (DV) and the primary outcome measure for all four research questions. Intellectus® statistics software was used to analyze data. The chi-square test of independence tool was used to compare variables. Other descriptive characteristics emerged. Binghamton University's Institutional Review Board approved this study.
Results: Primary objective results: χ2 = 4.08, df = 1, p = .043. Based on an alpha value of .05, the results were statistically significant. This research hypothesis suggests that clients who received one additional TCR three business days before their scheduled appointments had improved attendance compared to clients who received the clinic’s standard practice protocol of one TCR one business day before their scheduled appointments. Research question two results: χ2 = 17.20, df = 1, p < .001. The results were statistically significant based on an alpha value of .05. The research hypothesis suggests that appointment attendance will improve in clients who confirmed that they would attend their scheduled appointments than those who did not confirm that they would attend their scheduled appointments. Hence, a three-business-day TCR and a verbal commitment to attend the upcoming appointment may allow the client to make concrete plans to attend as scheduled. Research question three results: χ2 = 6.68, df = 2, p =.035. This supports a statistically significant relationship between primary SUD diagnosis type and appointment attendance variables based on an alpha value of .05. Hence, the hypothesis suggests that clients with a primary diagnosis of opioid use disorder (OUD) will have much-improved appointment attendance than those clients with the other primary SUD diagnosis types, specifically alcohol use disorder (AUD) and amphetamine use disorder (AMUD). Research question four results: χ2 = 0.08, df = 1, p = .776. Based on an alpha value of .05, the results indicate no statistically significant relationship between SUD diagnosis severity level and appointment attendance. Hence, no significant difference is noted between the observed and expected frequencies. The research hypothesis suggested that appointment attendance will improve in clients with severe SUD diagnosis levels than those with moderate SUD diagnosis levels, likely increasing their risk for disease progression. Demographic Data: the frequently observed race category was White (n = 291, 93.87%). The most observed category of assigned birth gender was Male (n = 175, 56.45%). The frequently observed age category was adult (30-39) (n = 129, 41.61%). The demographic data findings were consistent with the literature review. The demographic risk factors of opioid overdose death include male gender, individuals in the age range of 20 to 40 years old, and White non-Hispanic race (2). Compared to the same period the previous year, the attendance rate at the clinic improved by seven percent due to the additional TCR intervention.
Conclusion & Discussion: The study showed that using multiple TCRs to reach clients before their scheduled appointments will likely improve appointment attendance. The study emphasized that careful examination of demographic data can meaningfully impact the Clients’ SUD recovery path. The implication for practice should include identifying the risk factors necessary for healthcare professionals to individualize treatment, thereby optimizing health outcomes and equities. Also, SUD treatment clinics can implement multiple TCRs as an essential cue for clients to keep their appointments, likely maximizing the benefits of treatment and enhancing self-efficacy through decreasing relapse and overdose death rates. The study's strengths include using intervention and comparison groups and the statistically significant results of three research questions. The limitations of this study are the small sample size and the primary SUD diagnosis type, which only included the top three most frequently treated diagnoses at the clinic. Future research should focus on having a large sample size, allowing generalization of the findings. While this study's findings may be limited due to the sample size, it can provide insight into how SUD treatment clinics can improve appointment attendance among patients. These findings add to the body of research on decreasing missed appointments.
References:
1. Lagman, R. L., Samala, R. V., LeGrand, S., Parala-Metz, A., Patel, C., Neale, K., Carrino, C., Rybicki, L., Gamier, P., Mauk, M., & Nowak, M. (2020). “if you call them, they will come”: A telephone call reminder to decrease the no-show rate in an outpatient palliative medicine clinic. American Journal of Hospice and Palliative Medicine®, 38(5), 448–451. https://doi.org/10.1177/1049909120952322
2. Schiller, E. Y., Goyal, A., & Mechanic, O. J. (2017). Opioid Overdose. Retrieved October 26, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK470415/
3. Spithoff, S., & Kahan, M. (2015, June). Paradigm shift: Moving the management of alcohol use disorders from specialized care to primary care. Canadian Family Physician, 61, 491–493. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4463884/pdf/0610491.pdf
4. Tofighi, B., Grazioli, F., Bereket, S., Grossman, E., Aphinyanaphongs, Y., & Lee, J. (2017). Text message reminders for improving patient appointment adherence in an office-based buprenorphine program: A feasibility study. The American Journal on Addictions, 26(6), 581–586. https://doi.org/10.1111/ajad.12557
5. Youn, S., Geismar, H., & Pinedo, M. (2022). Planning and scheduling in healthcare for better care coordination: Current understanding, trending topics, and future opportunities. Production and Operations Management, 31(12), 4407–4423. https://doi.org/10.1111/poms.13867
Methods: This eight-week-long study used a quasi‐experimental design with intervention and comparison groups at an outpatient SUD treatment clinic in Broome County, New York. The intervention group received the three-business day TCR in addition to the clinic's standard protocol of one TCR to clients one business day before their scheduled appointments. The comparison group received the clinic’s standard protocol of one TCR. The primary research question: What is the relationship between one additional TCR three business days before clients’ appointments and attendance? Question 2: What is the relationship between appointment confirmation and attendance? Question 3: What is the relationship between SUD diagnosis type and appointment attendance? Question 4: What is the relationship between the SUD diagnosis severity level and appointment attendance? A convenient sample of 338 adult subjects were enrolled. After inclusion and exclusion criteria were applied, 310 subjects remained with 148 and 162 in the intervention and comparison groups, respectively. Appointment attendance was the dependent variable (DV) and the primary outcome measure for all four research questions. Intellectus® statistics software was used to analyze data. The chi-square test of independence tool was used to compare variables. Other descriptive characteristics emerged. Binghamton University's Institutional Review Board approved this study.
Results: Primary objective results: χ2 = 4.08, df = 1, p = .043. Based on an alpha value of .05, the results were statistically significant. This research hypothesis suggests that clients who received one additional TCR three business days before their scheduled appointments had improved attendance compared to clients who received the clinic’s standard practice protocol of one TCR one business day before their scheduled appointments. Research question two results: χ2 = 17.20, df = 1, p < .001. The results were statistically significant based on an alpha value of .05. The research hypothesis suggests that appointment attendance will improve in clients who confirmed that they would attend their scheduled appointments than those who did not confirm that they would attend their scheduled appointments. Hence, a three-business-day TCR and a verbal commitment to attend the upcoming appointment may allow the client to make concrete plans to attend as scheduled. Research question three results: χ2 = 6.68, df = 2, p =.035. This supports a statistically significant relationship between primary SUD diagnosis type and appointment attendance variables based on an alpha value of .05. Hence, the hypothesis suggests that clients with a primary diagnosis of opioid use disorder (OUD) will have much-improved appointment attendance than those clients with the other primary SUD diagnosis types, specifically alcohol use disorder (AUD) and amphetamine use disorder (AMUD). Research question four results: χ2 = 0.08, df = 1, p = .776. Based on an alpha value of .05, the results indicate no statistically significant relationship between SUD diagnosis severity level and appointment attendance. Hence, no significant difference is noted between the observed and expected frequencies. The research hypothesis suggested that appointment attendance will improve in clients with severe SUD diagnosis levels than those with moderate SUD diagnosis levels, likely increasing their risk for disease progression. Demographic Data: the frequently observed race category was White (n = 291, 93.87%). The most observed category of assigned birth gender was Male (n = 175, 56.45%). The frequently observed age category was adult (30-39) (n = 129, 41.61%). The demographic data findings were consistent with the literature review. The demographic risk factors of opioid overdose death include male gender, individuals in the age range of 20 to 40 years old, and White non-Hispanic race (2). Compared to the same period the previous year, the attendance rate at the clinic improved by seven percent due to the additional TCR intervention.
Conclusion & Discussion: The study showed that using multiple TCRs to reach clients before their scheduled appointments will likely improve appointment attendance. The study emphasized that careful examination of demographic data can meaningfully impact the Clients’ SUD recovery path. The implication for practice should include identifying the risk factors necessary for healthcare professionals to individualize treatment, thereby optimizing health outcomes and equities. Also, SUD treatment clinics can implement multiple TCRs as an essential cue for clients to keep their appointments, likely maximizing the benefits of treatment and enhancing self-efficacy through decreasing relapse and overdose death rates. The study's strengths include using intervention and comparison groups and the statistically significant results of three research questions. The limitations of this study are the small sample size and the primary SUD diagnosis type, which only included the top three most frequently treated diagnoses at the clinic. Future research should focus on having a large sample size, allowing generalization of the findings. While this study's findings may be limited due to the sample size, it can provide insight into how SUD treatment clinics can improve appointment attendance among patients. These findings add to the body of research on decreasing missed appointments.
References:
1. Lagman, R. L., Samala, R. V., LeGrand, S., Parala-Metz, A., Patel, C., Neale, K., Carrino, C., Rybicki, L., Gamier, P., Mauk, M., & Nowak, M. (2020). “if you call them, they will come”: A telephone call reminder to decrease the no-show rate in an outpatient palliative medicine clinic. American Journal of Hospice and Palliative Medicine®, 38(5), 448–451. https://doi.org/10.1177/1049909120952322
2. Schiller, E. Y., Goyal, A., & Mechanic, O. J. (2017). Opioid Overdose. Retrieved October 26, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK470415/
3. Spithoff, S., & Kahan, M. (2015, June). Paradigm shift: Moving the management of alcohol use disorders from specialized care to primary care. Canadian Family Physician, 61, 491–493. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4463884/pdf/0610491.pdf
4. Tofighi, B., Grazioli, F., Bereket, S., Grossman, E., Aphinyanaphongs, Y., & Lee, J. (2017). Text message reminders for improving patient appointment adherence in an office-based buprenorphine program: A feasibility study. The American Journal on Addictions, 26(6), 581–586. https://doi.org/10.1111/ajad.12557
5. Youn, S., Geismar, H., & Pinedo, M. (2022). Planning and scheduling in healthcare for better care coordination: Current understanding, trending topics, and future opportunities. Production and Operations Management, 31(12), 4407–4423. https://doi.org/10.1111/poms.13867
Learning Objectives:
- Discuss the negative impacts of missed appointments on patients in the outpatient substance use disorder treatment clinic setting.
- Identify the frequently cited reason for missed appointments at outpatient clinics.
- Determine the effectiveness of the intervention in improving appointment attendance.
