Back
(6) Scaling Up Low Barrier Wound Care for People who Use Drugs
Friday, April 25, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2

Jessica K. Lin
Undergraduate Student
University of Pennsylvania, Pennsylvania- ET
Eleanor Turi, PhD, RN, CCRN
Postdoctoral Fellow
University of Pennsylvania, Pennsylvania
Presenter(s)
Non-presenting author(s)
Background & Introduction: There is high demand for wound care among people who use drugs (PWUD), which has increased with the rise of xylazine in the opioid supply. Xylazine is an animal tranquilizer known to cause necrotic wounds (1). When wound care is delivered in hospitals, PWUD often experience stigma, discrimination, and limited pain and withdrawal management. There is a need for engaging, nonjudgmental approaches to delivering wound care for PWUD. Low barrier settings, defined as community-based care with flexible scheduling and harm reduction approaches (2), are associated with increased engagement and satisfaction with care among PWUD.
The current supply of low barrier wound care services does not meet the demand, as demonstrated by continuing rises in xylazine-associated chronic wounds that require hospitalization (3). Furthermore, PWUD have many health-related social needs such as unstable housing and food insecurity that complicate wound care delivery (4,5). Thus, multi-level factors likely influence outcomes among PWUD.
This study aims to identify determinants of and implementation strategies for scaling up low barrier wound care for PWUD. Systematically assessing how multiple systems of care and nested social and environmental interactions impact the delivery of low barrier wound care can help us uncover mechanisms for improving outcomes for this population.
Methods: This was a prospective sequential exploratory mixed methods study that included qualitative 1:1 interviews and community advisory board (CAB) meetings with an online survey. The interview guide was organized by the Consolidated Framework for Implementation Research (CFIR) 2.0. Outcomes include a comprehensive list of determinants, matched implementation strategies, and CAB ratings of acceptability, feasibility, and appropriateness of strategies, measured by the Acceptability of Intervention Measure, Feasibility of Intervention Measure, and Appropriateness of Intervention Measure.
Low barrier wound care was defined as care offered in organizations with walk-in services, harm reduction approaches, and flexible hours. Interviews and CAB meetings were conducted via Zoom. Participants were included if they were wound care administrators, providers, or recovery specialists from Philadelphia, Pennsylvania or surrounding regions given the high contamination of xylazine in the regional drug supply. Convenience and snowball sampling approaches were used.
Qualitative data was analyzed in Dedoose software by two independent coders, using deductive CFIR and inductive codes. Codes were organized into deductive CFIR themes. We analyzed CAB survey results in Excel and provide descriptive statistics.
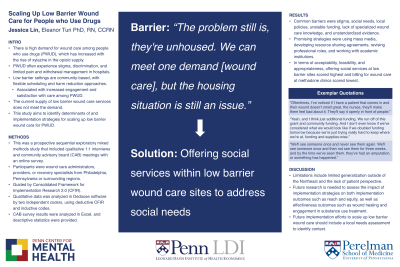
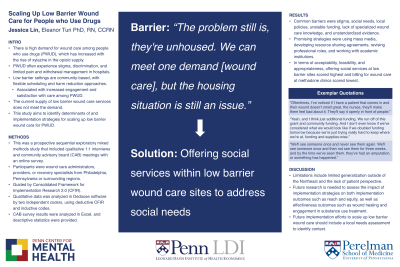
Results: Common barriers to scaling up low barrier wound care include stigma, social needs, local policies, unstable funding, lack of specialized wound care knowledge, and unstandardized evidence. The stigma PWUD face prevents them from seeking out medical treatment and staying consistent throughout the course of their treatment. Housing was the most identified social needs barrier that impacts the provision of low barrier wound care. Participants reported that housing impacts patients’ ability to keep their wounds clean as well as their access to wound care supplies. Policies against harm reduction control funding for low barrier wound care organizations and contribute to the movement of patients into settings such as jails, where wound care is low quality. Participants wished for more funding to be able to scale their services, provide more consistent care, and buy needed but costly supplies instead of rationing and storing their supplies in basements. Participants reported learning wound care from various sources with varied quality, including city guidelines, wound care learning events put on by philanthropies, or on the job. This can lead to inconsistencies in how wound care is provided. There is some disagreement in the community about who should and should not be delivering care in the community, as well as how they should be educated.
Promising examples of outer setting strategies with clinical or practical application include using social media to address stigma and foster networking, innovations to track patients across settings, and having a centralized department for wound care resources. Strategies that targeted inner setting factors included accessing new funding and changing the physical structure of sites and equipment. Common individual level evidence-based strategies included revising professional roles, shadowing other experts, and involving patients/consumers and family members in care. Promoting the adaptability of the innovation is another evidence-based strategy that can help promote the uptake and sustainability of low barrier wound care. Strategies that targeted the innovation domain included using advisory boards and workgroups, developing academic partnerships, and conducting local consensus discussions. In terms of the CAB survey results, offering social services at low barrier sites scored highest for acceptability, feasibility, and appropriateness, while billing for wound care at methadone clinics scored lowest.
Conclusion & Discussion: This study comprehensively assessed determinants of and implementation strategies for scaling up low barrier wound care services for people who use drugs. It blended theory, literature, and community partnered perspectives.
Future implementation efforts to scale up low barrier wound care should include a local needs assessment to identify context, then pull in implementation strategies from our results that are most promising to addressing barriers and priorities. Future research is needed to assess the impact of implementation strategies on both implementation outcomes such as reach and equity, as well as effectiveness outcomes such as wound healing and engagement in substance use treatment.
Our study has limitations, including limited generalization outside of the Northeast, a hotspot of the xylazine crisis with a unique harm reduction culture. Also, our study focused on analyzing system-level barriers to low barrier wound care implementation; therefore, PWUD were not included in our sample. The patient perspective will be included in future studies that test effectiveness and implementation.
References: 1. Substance Use Philly. (2023). Xylazine. Retrieved September 27th, 2023 from https://www.substanceusephilly.com/tranq
2. Jakubowski, A., & Fox, A. (2020). Defining low-threshold buprenorphine treatment. J Addict Med, 14(2), 95-98. https://doi.org/10.1097/adm.0000000000000555
3. Soderquist, M., Delgado, G., Abdelfattah, H., Thoder, J., & Solarz, M. (2023). Necrotic upper-extremity infections in people who inject drugs: A case series. J Hand Surg Am. https://doi.org/10.1016/j.jhsa.2023.04.001
4. Raja, A., Heeren, T. C., Walley, A. Y., Winter, M. R., Mesic, A., & Saitz, R. (2022). Food Insecurity and Substance use in People with HIV Infection and Substance use Disorder. Substance Abuse, 43(1), 104-112. https://doi.org/10.1080/08897077.2020.1748164
5. Substance Abuse and Mental Health Services Administration. (2023). Addressing Social Determinants of Health Among Individuals Experiencing Homelessness. https://www.samhsa.gov/blog/addressing-social-determinants-health-among-individuals-experiencing-homelessness
The current supply of low barrier wound care services does not meet the demand, as demonstrated by continuing rises in xylazine-associated chronic wounds that require hospitalization (3). Furthermore, PWUD have many health-related social needs such as unstable housing and food insecurity that complicate wound care delivery (4,5). Thus, multi-level factors likely influence outcomes among PWUD.
This study aims to identify determinants of and implementation strategies for scaling up low barrier wound care for PWUD. Systematically assessing how multiple systems of care and nested social and environmental interactions impact the delivery of low barrier wound care can help us uncover mechanisms for improving outcomes for this population.
Methods: This was a prospective sequential exploratory mixed methods study that included qualitative 1:1 interviews and community advisory board (CAB) meetings with an online survey. The interview guide was organized by the Consolidated Framework for Implementation Research (CFIR) 2.0. Outcomes include a comprehensive list of determinants, matched implementation strategies, and CAB ratings of acceptability, feasibility, and appropriateness of strategies, measured by the Acceptability of Intervention Measure, Feasibility of Intervention Measure, and Appropriateness of Intervention Measure.
Low barrier wound care was defined as care offered in organizations with walk-in services, harm reduction approaches, and flexible hours. Interviews and CAB meetings were conducted via Zoom. Participants were included if they were wound care administrators, providers, or recovery specialists from Philadelphia, Pennsylvania or surrounding regions given the high contamination of xylazine in the regional drug supply. Convenience and snowball sampling approaches were used.
Qualitative data was analyzed in Dedoose software by two independent coders, using deductive CFIR and inductive codes. Codes were organized into deductive CFIR themes. We analyzed CAB survey results in Excel and provide descriptive statistics.
Results: Common barriers to scaling up low barrier wound care include stigma, social needs, local policies, unstable funding, lack of specialized wound care knowledge, and unstandardized evidence. The stigma PWUD face prevents them from seeking out medical treatment and staying consistent throughout the course of their treatment. Housing was the most identified social needs barrier that impacts the provision of low barrier wound care. Participants reported that housing impacts patients’ ability to keep their wounds clean as well as their access to wound care supplies. Policies against harm reduction control funding for low barrier wound care organizations and contribute to the movement of patients into settings such as jails, where wound care is low quality. Participants wished for more funding to be able to scale their services, provide more consistent care, and buy needed but costly supplies instead of rationing and storing their supplies in basements. Participants reported learning wound care from various sources with varied quality, including city guidelines, wound care learning events put on by philanthropies, or on the job. This can lead to inconsistencies in how wound care is provided. There is some disagreement in the community about who should and should not be delivering care in the community, as well as how they should be educated.
Promising examples of outer setting strategies with clinical or practical application include using social media to address stigma and foster networking, innovations to track patients across settings, and having a centralized department for wound care resources. Strategies that targeted inner setting factors included accessing new funding and changing the physical structure of sites and equipment. Common individual level evidence-based strategies included revising professional roles, shadowing other experts, and involving patients/consumers and family members in care. Promoting the adaptability of the innovation is another evidence-based strategy that can help promote the uptake and sustainability of low barrier wound care. Strategies that targeted the innovation domain included using advisory boards and workgroups, developing academic partnerships, and conducting local consensus discussions. In terms of the CAB survey results, offering social services at low barrier sites scored highest for acceptability, feasibility, and appropriateness, while billing for wound care at methadone clinics scored lowest.
Conclusion & Discussion: This study comprehensively assessed determinants of and implementation strategies for scaling up low barrier wound care services for people who use drugs. It blended theory, literature, and community partnered perspectives.
Future implementation efforts to scale up low barrier wound care should include a local needs assessment to identify context, then pull in implementation strategies from our results that are most promising to addressing barriers and priorities. Future research is needed to assess the impact of implementation strategies on both implementation outcomes such as reach and equity, as well as effectiveness outcomes such as wound healing and engagement in substance use treatment.
Our study has limitations, including limited generalization outside of the Northeast, a hotspot of the xylazine crisis with a unique harm reduction culture. Also, our study focused on analyzing system-level barriers to low barrier wound care implementation; therefore, PWUD were not included in our sample. The patient perspective will be included in future studies that test effectiveness and implementation.
References: 1. Substance Use Philly. (2023). Xylazine. Retrieved September 27th, 2023 from https://www.substanceusephilly.com/tranq
2. Jakubowski, A., & Fox, A. (2020). Defining low-threshold buprenorphine treatment. J Addict Med, 14(2), 95-98. https://doi.org/10.1097/adm.0000000000000555
3. Soderquist, M., Delgado, G., Abdelfattah, H., Thoder, J., & Solarz, M. (2023). Necrotic upper-extremity infections in people who inject drugs: A case series. J Hand Surg Am. https://doi.org/10.1016/j.jhsa.2023.04.001
4. Raja, A., Heeren, T. C., Walley, A. Y., Winter, M. R., Mesic, A., & Saitz, R. (2022). Food Insecurity and Substance use in People with HIV Infection and Substance use Disorder. Substance Abuse, 43(1), 104-112. https://doi.org/10.1080/08897077.2020.1748164
5. Substance Abuse and Mental Health Services Administration. (2023). Addressing Social Determinants of Health Among Individuals Experiencing Homelessness. https://www.samhsa.gov/blog/addressing-social-determinants-health-among-individuals-experiencing-homelessness
Learning Objectives:
- Upon completion, participant will be able to define low barrier wound care.
- Upon completion, participant will be able to identify barriers to scaling up low barrier wound care.
- Upon completion, participant will be able to assess implementation strategies for improving low barrier wound care.
