Back
Award Winner - Associated Professional
(11) Harm Reduction Vending Machines Increase Equitable Access to Naloxone and Health Supplies
Friday, April 25, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2
- AH
Ashleigh N. Herrera, PhD, LCSW
Assistant Professor
California State University, Bakersfield, California
Presenter(s)
Background & Introduction: Despite the need for equitable access to harm reduction services, people who use drugs (PWUD), especially those with multiple vulnerabilities, experience a multitude of barriers to accessing harm reduction services and retaining harm reduction supplies, including naloxone (Kinnard et al., 2021; Tobin et al., 2018). In response to national and local trends in drug overdose and HCV and HIV infection rates, cities across the United States have begun to implement harm reduction vending machines (HVRMs), which have been adopted in Europe since the 1980s. However, no known studies to date have addressed community based HRVM reach and effectiveness in harm reduction supply access and decreasing health disparities among racial and ethnic minorities, persons experiencing homelessness (PEH), and justice involved (JI) individuals. Given the ongoing opioid epidemic which has been exacerbated by the proliferation of synthetic opioids and led to recent acceleration in mortality rates for Black, Latine, PEH, and JI populations, (CDC, 2023; LACDP, 2023; Mital et al., 2020; NIDA, 2023; Pew Research Center, 2022; Townsend et al., 2022) this study aims to examine characteristics of people who utilize the HRVM program in terms of risk of drug-related morbidity and mortality and in terms of race/ethnicity, housing status, and justice-involvement.
Methods: Using a targeted sampling approach, the research team recruited, registered, and conducted a brief cross-sectional survey with 133 participants for an HRVM located outside a county mental health clinic in Bakersfield, California, during a 5-month period. As each participant was assigned a unique ID number to access the HRVM, longitudinal secondary data on participants’ utilization and dispensation rates of specific supplies, including naloxone, was obtained. Descriptive statistics were conducted to examine characteristics of individuals utilizing the HRVM program. To investigate the association between participants’ racial/ethnic identity (“minoritized group” vs. “non-minoritized group”) and HRVM utilization (“yes” or “no”), a chi-square test of independence was performed. Similarly, chi-square tests of independence were conducted for participants’ gender (“male” or “not male”) and HRVM utilization and naloxone dispensation; participants’ risk for opioid overdose (“high” vs. “low”) and safer substance use supply dispensation and HRVM utilization. The hypotheses include: 1) participants from minoritized groups will be more likely to access the HRVM than non-minoritized groups, 2) female participants will be more likely to access the HRVM than male participants, and 3) participants at high-risk of overdose will be more likely to access the HRVM and safer substance use supplies than low risk participants.
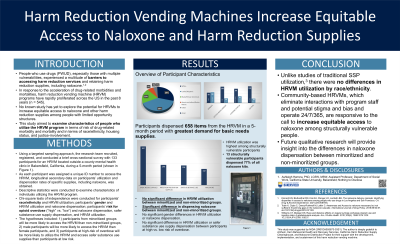
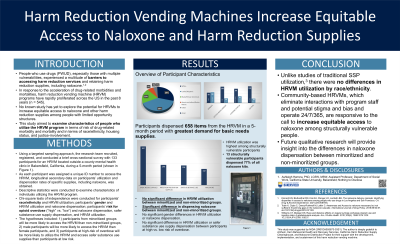
Results: A total of 133 participants who completed the brief-cross sectional survey were included in the final analytic sample. Slightly over half of the participants were female (51.1%). Racial demographics included Hispanic (38.5%), non-Hispanic White (28.9%), non-Hispanic Black (20%), American Indian and Alaska Native (7.4%), Other (5%), and Asian (1%). While most participants reported residing in housing they owned or rented (44.5%), almost a third reported that they were experiencing either sheltered (n = 14) or unsheltered homelessness (n =29). The median age was 40 years old (IQR: 30-51). Almost one-quarter of participants (n =30) reported past 12-month history of CJI.
During the past 5 months, registered participants dispensed 658 items from the HRVM. While basic needs supplies (e.g. hygiene and menstrual hygiene kits) were in highest demand (n =267), participants also obtained infection prevention supplies (e.g. condoms and wound care kits) (n =140), safer substance use supplies (e.g. safer injection and sharps disposal kits) (n =136), and naloxone (n =112). Among structurally vulnerable participants, almost 40% of participants at high risk of overdose used the HRVM after registration as well as 47% of justice-involved participants, 50% of persons experiencing sheltered homelessness, 45% of PEUH, and 60% of participants who recently were in institutional settings. Furthermore, 13 structurally vulnerable participants dispensed 77% of all naloxone kits (range 1 – 37 naloxone kits).
A chi-square test revealed no significant difference in utilizing the HRVM between minoritized and non-minoritized groups, X2 (1, N = 133) = 3.40, p = .065. However, a chi-square test revealed a significant difference in dispensing naloxone from the HRVM between minoritized and non-minoritized groups, X2 (1, N = 133) = 6.796, p = .009. Similarly, a chi-square test revealed no significant difference in utilizing the HRVM between genders, X2 (1, N = 133) = 0.640, p = .424, nor any significant difference in dispensing naloxone from the HRVM between genders, X2 (1, N = 133) = 0.406, p = .524. Finally, a chi-square test revealed no significant difference in HRVM access by risk level for overdose, X2 (1, N = 133) = .201, p = .654; and no significant difference in safer substance use supply access from the HRVM by risk level for overdose, X2 (1, N = 133) = .016, p = .900.
Conclusion & Discussion: While previous studies found racial disparities in SSP utilization (Williams & Metzger, 2010), the present study did not find any significant differences in HRVM utilization by race/ethnicity. However, like previous studies reporting racial disparities in naloxone distribution at SSPs (Kinnard et al., 2021) and racial disparities in the naloxone cascade (Khan et al., 2023; Ward et al., 2024), the present study also found a significant difference in naloxone dispensation from the HRVM by race/ethnicity with non-minoritized participants being more likely to dispense naloxone than minoritized participants. Multiple studies have found that females were more likely to consistently possess naloxone (Madah-Amiri et al., 2019; Ward et al., 2024), but the present study did not find a significant difference in naloxone dispensation by gender. Like previous studies that found similar SSP utilization between genders, there were no significant differences in HRVM utilization by gender. Of particular note, HRVM utilization and safer substance use dispensation did not significantly differ between high- and low-risk participants. Community-based HRVMs, which eliminate interactions with program staff and potential stigma and bias and operate 24/7/365, are responsive to the call to increase equitable access to naloxone among structurally vulnerable people, including PEH, JI persons, and minoritized groups.
References: Centers for Disease Control and Prevention. Drug Overdose Deaths. Published August 23, 2023. Accessed November 6, 2023. https://www.cdc.gov/drugoverdose/deaths/index.html
Centers for Disease Control and Prevention. Summary of information of the safety and effectiveness of syringe service programs (SSPs). Updated January 11, 2023. Accessed June 14, 2023. https://www.cdc.gov/ssp/syringe-services-programs-summary.html
Kinnard, E.N., Bluthenthal, R.N., Kral, A.H., Wenger, L.D., & Lambdin, B.H. (2021). The naloxone delivery cascade: Identifying disparities in access to naloxone among people who use drugs in Los Angeles and San Francisco, CA. Drug & Alcohol Dependence, 225(108759).
Los Angeles County Department of Public Health. New Public Health Report Shows Sharp Rise in Mortality Among People Experiencing Homelessness – Increase Driven by Fentanyl-Related Deaths, Traffic Deaths, and Homicides. Published on May 12, 2023. Accessed on November 6, 2023.
https://publichealth.lacounty.gov/phcommon/public/media/mediapubhpdetail.cfm?prid=4384
Mital, S., Wolff, J., & Carroll, J.J. (2020). The Relationship Between Incarceration History and Overdose in North America: A Scoping Review of the Evidence. Drug Alcohol Dependence;213:108088. doi:10.1016/j.drugalcdep.2020.108088
National Institute on Drug Abuse. Drug Overdose Death Rates. Published June 30, 2023. Accessed November 6, 2023. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
Pew Research Center. Recent Survey in US Drug Overdose Deaths Has Hit Black Men the Hardest. Published 19, 2022. Accessed November 6, 2023. https://www.pewresearch.org/shortreads/2022/01/19/recent-surge-in-u-s-drug-overdose-deaths-has-hit-black-men-the-hardest/
Tobin, K., Clyde, C., Davey-Rothwell, M., & Latkin, C. (2018). Awareness and Access to naloxone necessary but not sufficient: Examining gaps in the naloxone cascade. International Journal of Drug Policy, 59:94-97. doi:10/1016/j.drugpo/2018.07.003
Townsend, T., Kline, D., Rivera-Aguirre, A., Bunting, A.M., Mauro, P.M., Marshall, B.D.L., Martin, S.S., & Cerda, M. (2022) Racial/Ethnic and Geographic Trend in Combined Stimulant/Opioid Overdoses, 2007-2019. American Journal of Epidemiology, 191(4):599-612. doi.org/10.1093/aje/kwab290
Williams, C.T., & Metzger, D.S. (2010). Race and distance effects on regular syringe exchange program use and injection risks: A geobehavioral analysis. Am J Public Health, 100(6): 1068-1074. DOI: 10.2105/AJPH.2008.158337.
Methods: Using a targeted sampling approach, the research team recruited, registered, and conducted a brief cross-sectional survey with 133 participants for an HRVM located outside a county mental health clinic in Bakersfield, California, during a 5-month period. As each participant was assigned a unique ID number to access the HRVM, longitudinal secondary data on participants’ utilization and dispensation rates of specific supplies, including naloxone, was obtained. Descriptive statistics were conducted to examine characteristics of individuals utilizing the HRVM program. To investigate the association between participants’ racial/ethnic identity (“minoritized group” vs. “non-minoritized group”) and HRVM utilization (“yes” or “no”), a chi-square test of independence was performed. Similarly, chi-square tests of independence were conducted for participants’ gender (“male” or “not male”) and HRVM utilization and naloxone dispensation; participants’ risk for opioid overdose (“high” vs. “low”) and safer substance use supply dispensation and HRVM utilization. The hypotheses include: 1) participants from minoritized groups will be more likely to access the HRVM than non-minoritized groups, 2) female participants will be more likely to access the HRVM than male participants, and 3) participants at high-risk of overdose will be more likely to access the HRVM and safer substance use supplies than low risk participants.
Results: A total of 133 participants who completed the brief-cross sectional survey were included in the final analytic sample. Slightly over half of the participants were female (51.1%). Racial demographics included Hispanic (38.5%), non-Hispanic White (28.9%), non-Hispanic Black (20%), American Indian and Alaska Native (7.4%), Other (5%), and Asian (1%). While most participants reported residing in housing they owned or rented (44.5%), almost a third reported that they were experiencing either sheltered (n = 14) or unsheltered homelessness (n =29). The median age was 40 years old (IQR: 30-51). Almost one-quarter of participants (n =30) reported past 12-month history of CJI.
During the past 5 months, registered participants dispensed 658 items from the HRVM. While basic needs supplies (e.g. hygiene and menstrual hygiene kits) were in highest demand (n =267), participants also obtained infection prevention supplies (e.g. condoms and wound care kits) (n =140), safer substance use supplies (e.g. safer injection and sharps disposal kits) (n =136), and naloxone (n =112). Among structurally vulnerable participants, almost 40% of participants at high risk of overdose used the HRVM after registration as well as 47% of justice-involved participants, 50% of persons experiencing sheltered homelessness, 45% of PEUH, and 60% of participants who recently were in institutional settings. Furthermore, 13 structurally vulnerable participants dispensed 77% of all naloxone kits (range 1 – 37 naloxone kits).
A chi-square test revealed no significant difference in utilizing the HRVM between minoritized and non-minoritized groups, X2 (1, N = 133) = 3.40, p = .065. However, a chi-square test revealed a significant difference in dispensing naloxone from the HRVM between minoritized and non-minoritized groups, X2 (1, N = 133) = 6.796, p = .009. Similarly, a chi-square test revealed no significant difference in utilizing the HRVM between genders, X2 (1, N = 133) = 0.640, p = .424, nor any significant difference in dispensing naloxone from the HRVM between genders, X2 (1, N = 133) = 0.406, p = .524. Finally, a chi-square test revealed no significant difference in HRVM access by risk level for overdose, X2 (1, N = 133) = .201, p = .654; and no significant difference in safer substance use supply access from the HRVM by risk level for overdose, X2 (1, N = 133) = .016, p = .900.
Conclusion & Discussion: While previous studies found racial disparities in SSP utilization (Williams & Metzger, 2010), the present study did not find any significant differences in HRVM utilization by race/ethnicity. However, like previous studies reporting racial disparities in naloxone distribution at SSPs (Kinnard et al., 2021) and racial disparities in the naloxone cascade (Khan et al., 2023; Ward et al., 2024), the present study also found a significant difference in naloxone dispensation from the HRVM by race/ethnicity with non-minoritized participants being more likely to dispense naloxone than minoritized participants. Multiple studies have found that females were more likely to consistently possess naloxone (Madah-Amiri et al., 2019; Ward et al., 2024), but the present study did not find a significant difference in naloxone dispensation by gender. Like previous studies that found similar SSP utilization between genders, there were no significant differences in HRVM utilization by gender. Of particular note, HRVM utilization and safer substance use dispensation did not significantly differ between high- and low-risk participants. Community-based HRVMs, which eliminate interactions with program staff and potential stigma and bias and operate 24/7/365, are responsive to the call to increase equitable access to naloxone among structurally vulnerable people, including PEH, JI persons, and minoritized groups.
References: Centers for Disease Control and Prevention. Drug Overdose Deaths. Published August 23, 2023. Accessed November 6, 2023. https://www.cdc.gov/drugoverdose/deaths/index.html
Centers for Disease Control and Prevention. Summary of information of the safety and effectiveness of syringe service programs (SSPs). Updated January 11, 2023. Accessed June 14, 2023. https://www.cdc.gov/ssp/syringe-services-programs-summary.html
Kinnard, E.N., Bluthenthal, R.N., Kral, A.H., Wenger, L.D., & Lambdin, B.H. (2021). The naloxone delivery cascade: Identifying disparities in access to naloxone among people who use drugs in Los Angeles and San Francisco, CA. Drug & Alcohol Dependence, 225(108759).
Los Angeles County Department of Public Health. New Public Health Report Shows Sharp Rise in Mortality Among People Experiencing Homelessness – Increase Driven by Fentanyl-Related Deaths, Traffic Deaths, and Homicides. Published on May 12, 2023. Accessed on November 6, 2023.
https://publichealth.lacounty.gov/phcommon/public/media/mediapubhpdetail.cfm?prid=4384
Mital, S., Wolff, J., & Carroll, J.J. (2020). The Relationship Between Incarceration History and Overdose in North America: A Scoping Review of the Evidence. Drug Alcohol Dependence;213:108088. doi:10.1016/j.drugalcdep.2020.108088
National Institute on Drug Abuse. Drug Overdose Death Rates. Published June 30, 2023. Accessed November 6, 2023. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates
Pew Research Center. Recent Survey in US Drug Overdose Deaths Has Hit Black Men the Hardest. Published 19, 2022. Accessed November 6, 2023. https://www.pewresearch.org/shortreads/2022/01/19/recent-surge-in-u-s-drug-overdose-deaths-has-hit-black-men-the-hardest/
Tobin, K., Clyde, C., Davey-Rothwell, M., & Latkin, C. (2018). Awareness and Access to naloxone necessary but not sufficient: Examining gaps in the naloxone cascade. International Journal of Drug Policy, 59:94-97. doi:10/1016/j.drugpo/2018.07.003
Townsend, T., Kline, D., Rivera-Aguirre, A., Bunting, A.M., Mauro, P.M., Marshall, B.D.L., Martin, S.S., & Cerda, M. (2022) Racial/Ethnic and Geographic Trend in Combined Stimulant/Opioid Overdoses, 2007-2019. American Journal of Epidemiology, 191(4):599-612. doi.org/10.1093/aje/kwab290
Williams, C.T., & Metzger, D.S. (2010). Race and distance effects on regular syringe exchange program use and injection risks: A geobehavioral analysis. Am J Public Health, 100(6): 1068-1074. DOI: 10.2105/AJPH.2008.158337.
Learning Objectives:
- Describe the impact of HRVM programs on promoting equitable access to naloxone.
- Describe the impact of HRVM programs on promoting equitable access to harm reduction supplies.
- Discuss the benefits of including basic needs supplies in HRVM program product offerings to increase engagement and decrease stigma associated with HRVM program use.
