Back

(117) Treating Opioid Use Disorder: Perspective of FQHC Clinicians in Los Angeles
Saturday, April 26, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2
Has Audio

Andrew Schmidt, BS, ME
Medical Student
Kaiser Permanente School of Medicine, California
Kurtis Pruitt, BS
Medical Student
Kaiser Permanente School of Medicine, California
Presenter(s)
Background & Introduction: The opioid epidemic, driven by shifts in pain management practices, patient expectations, and provider behaviors, has led to widespread opioid overprescription and a significant underestimation of addiction risks [1]. This crisis remains a critical public health concern, particularly in regions like Los Angeles County, which reported over 1,700 opioid-related deaths last year [2,3]. In response to the growing epidemic, the Drug Enforcement Administration (DEA) mandated all registrants to complete continuing medical education (CME) on medication-assisted treatment (MAT) for opioid use disorder (OUD) in 2023. However, gaps remain in understanding the impact of such interventions on clinical practice.
Venice Family Clinic (VFC), a community health care center serving Los Angeles, recently merged with South Bay Family Health Care, prompting a reassessment of its OUD management strategies. This study aims to assess VFC clinicians' confidence in treating OUD patients and utilizing MAT, the perceived effectiveness of the mandated CME training, and the key barriers and resources in the OUD treatment landscape. By addressing these emerging issues, we seek to provide insights into optimizing OUD care within community health settings.
Methods: A cross-sectional survey was developed and distributed to all clinicians at VFC locations in South Bay, Los Angeles, designed to evaluate key aspects of OUD management. The survey comprised two main sections:
The first section assessed whether clinicians were providers of MAT, their completion of the newly mandated CME, and the frequency with which they encountered patients with OUD. Clinicians were also asked to self-evaluate their confidence in treating OUD patients and their understanding of current OUD treatment guidelines. Bivariate analysis was conducted to explore associations between these self-reported factors, aiming to identify patterns and relationships between clinical practices, education, and clinician confidence in OUD management.
In the second section, the survey focused on resources and barriers. Clinicians were asked to report which resources they found most effective in treating patients with OUD, and to identify the most common barriers they face in providing care. The frequency of responses for these items was tallied to highlight the most prevalent challenges and support needs within the clinic's OUD treatment landscape.
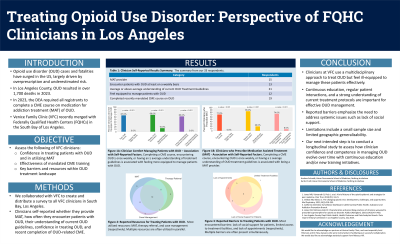
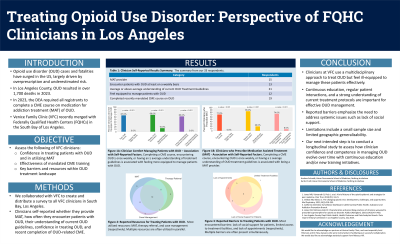
Results: Out of 33 physician respondents, 45% reported prescribing MAT for OUD, and 39% encountered OUD patients weekly. While 59% felt they possessed at least an average understanding of current OUD treatment guidelines, only 36% believed they were adequately equipped to manage OUD patients. Additionally, 64% had completed the recently mandated CME on opioid prescriptions and OUD management. The most commonly used resources to treat OUD were medication-assisted treatment (MAT) (58% of respondents) and outpatient therapy referrals (55% of respondents). The most commonly reported patient-related barrier to treatment was noncompliance (39% of respondents), while limited access to treatment facilities was the most cited resource-related barrier (58% of respondents).
In the bivariate analysis, providers who encountered OUD patients weekly were significantly more likely to prescribe MAT, felt better equipped to manage OUD patients, and had a greater knowledge of treatment guidelines (p < 0.05). Providers who completed mandated CME courses reported feeling more confident in managing OUD patients and had better knowledge of OUD treatment guidelines (p < 0.001). Furthermore, those with at least an average understanding of OUD treatment guidelines were significantly more likely to feel equipped to manage OUD patients (p < 0.001).
Conclusion & Discussion: Our findings highlight the significant role that clinician education and frequent interactions with OUD patients play in improving treatment outcomes. Clinicians who completed CME training and regularly encountered OUD patients were more likely to prescribe MAT and felt better equipped to manage OUD. These results underscore the need for ongoing, targeted education to enhance clinician competence in OUD management.
An additional finding is the identification of systemic barriers, including limited access to treatment facilities and patient noncompliance, which clinicians consistently cited as obstacles. These challenges call for a broader, system-level approach to improving OUD treatment infrastructure. Importantly, our findings may inform policy, as recent studies show physicians do not prescribe MAT near their authorized limits, highlighting a missed opportunity for broader utilization [4].
While Venice Family Clinic (VFC) employs a multidisciplinary approach, many clinicians still feel inadequately equipped to manage OUD patients. This suggests training alone is insufficient without addressing external factors like resource availability and patient engagement. Limitations include a small sample size and limited generalizability. Future studies should explore the link between clinician training, system-level barriers, and patient outcomes across healthcare settings.
References: 1. Jones, M. R., Viswanath, O., Peck, J., Kaye, A. D., Gill, J. S., & Simopoulos, T. T. (2018). A Brief History of the Opioid Epidemic and Strategies for Pain Medicine. Pain and therapy, 7(1), 13–21.
2. Volkow, N. D., & Blanco, C. (2021). The changing opioid crisis: development, challenges and opportunities. Molecular psychiatry, 26(1), 218–233.
3. California Overdose Surveillance Dashboard. California Department of Public Health - Substance and Addiction Prevention Branch.
4. Jones, C. M., & McCance-Katz, E. F. (2019). Characteristics and prescribing practices of clinicians recently waivered to prescribe buprenorphine for the treatment of opioid use disorder. Addiction (Abingdon, England), 114(3), 471–482.
5. Data Report: Fentanyl Overdoses in Los Angeles County. Health Outcomes and Data Analytics Branch, Substance Abuse Prevention and Control, Los Angeles County Department of Public Health, July 2024.
Venice Family Clinic (VFC), a community health care center serving Los Angeles, recently merged with South Bay Family Health Care, prompting a reassessment of its OUD management strategies. This study aims to assess VFC clinicians' confidence in treating OUD patients and utilizing MAT, the perceived effectiveness of the mandated CME training, and the key barriers and resources in the OUD treatment landscape. By addressing these emerging issues, we seek to provide insights into optimizing OUD care within community health settings.
Methods: A cross-sectional survey was developed and distributed to all clinicians at VFC locations in South Bay, Los Angeles, designed to evaluate key aspects of OUD management. The survey comprised two main sections:
The first section assessed whether clinicians were providers of MAT, their completion of the newly mandated CME, and the frequency with which they encountered patients with OUD. Clinicians were also asked to self-evaluate their confidence in treating OUD patients and their understanding of current OUD treatment guidelines. Bivariate analysis was conducted to explore associations between these self-reported factors, aiming to identify patterns and relationships between clinical practices, education, and clinician confidence in OUD management.
In the second section, the survey focused on resources and barriers. Clinicians were asked to report which resources they found most effective in treating patients with OUD, and to identify the most common barriers they face in providing care. The frequency of responses for these items was tallied to highlight the most prevalent challenges and support needs within the clinic's OUD treatment landscape.
Results: Out of 33 physician respondents, 45% reported prescribing MAT for OUD, and 39% encountered OUD patients weekly. While 59% felt they possessed at least an average understanding of current OUD treatment guidelines, only 36% believed they were adequately equipped to manage OUD patients. Additionally, 64% had completed the recently mandated CME on opioid prescriptions and OUD management. The most commonly used resources to treat OUD were medication-assisted treatment (MAT) (58% of respondents) and outpatient therapy referrals (55% of respondents). The most commonly reported patient-related barrier to treatment was noncompliance (39% of respondents), while limited access to treatment facilities was the most cited resource-related barrier (58% of respondents).
In the bivariate analysis, providers who encountered OUD patients weekly were significantly more likely to prescribe MAT, felt better equipped to manage OUD patients, and had a greater knowledge of treatment guidelines (p < 0.05). Providers who completed mandated CME courses reported feeling more confident in managing OUD patients and had better knowledge of OUD treatment guidelines (p < 0.001). Furthermore, those with at least an average understanding of OUD treatment guidelines were significantly more likely to feel equipped to manage OUD patients (p < 0.001).
Conclusion & Discussion: Our findings highlight the significant role that clinician education and frequent interactions with OUD patients play in improving treatment outcomes. Clinicians who completed CME training and regularly encountered OUD patients were more likely to prescribe MAT and felt better equipped to manage OUD. These results underscore the need for ongoing, targeted education to enhance clinician competence in OUD management.
An additional finding is the identification of systemic barriers, including limited access to treatment facilities and patient noncompliance, which clinicians consistently cited as obstacles. These challenges call for a broader, system-level approach to improving OUD treatment infrastructure. Importantly, our findings may inform policy, as recent studies show physicians do not prescribe MAT near their authorized limits, highlighting a missed opportunity for broader utilization [4].
While Venice Family Clinic (VFC) employs a multidisciplinary approach, many clinicians still feel inadequately equipped to manage OUD patients. This suggests training alone is insufficient without addressing external factors like resource availability and patient engagement. Limitations include a small sample size and limited generalizability. Future studies should explore the link between clinician training, system-level barriers, and patient outcomes across healthcare settings.
References: 1. Jones, M. R., Viswanath, O., Peck, J., Kaye, A. D., Gill, J. S., & Simopoulos, T. T. (2018). A Brief History of the Opioid Epidemic and Strategies for Pain Medicine. Pain and therapy, 7(1), 13–21.
2. Volkow, N. D., & Blanco, C. (2021). The changing opioid crisis: development, challenges and opportunities. Molecular psychiatry, 26(1), 218–233.
3. California Overdose Surveillance Dashboard. California Department of Public Health - Substance and Addiction Prevention Branch.
4. Jones, C. M., & McCance-Katz, E. F. (2019). Characteristics and prescribing practices of clinicians recently waivered to prescribe buprenorphine for the treatment of opioid use disorder. Addiction (Abingdon, England), 114(3), 471–482.
5. Data Report: Fentanyl Overdoses in Los Angeles County. Health Outcomes and Data Analytics Branch, Substance Abuse Prevention and Control, Los Angeles County Department of Public Health, July 2024.
Learning Objectives:
- Upon completion, participants will be able to describe how continuing medical education (CME) on medication-assisted treatment (MAT) influences clinician confidence and competence in managing opioid use disorder (OUD).
- Upon completion, participants will be able to identify the most common barriers clinicians face in treating opioid use disorder (OUD), including patient noncompliance and limited access to treatment facilities.
- Upon completion, participants will be able to analyze the relationship between clinician interactions with OUD patients and their likelihood of prescribing medication-assisted treatment (MAT).
