Back
(16) Recovery Capital among Patients Receiving Buprenorphine Treatment for Opioid Use Disorder
Friday, April 25, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2
- CR
Christopher Rowe, PhD
Director of Research and Population Health
Ophelia Health, Inc., New York 
Adam M. Bisaga, MD
Professor
Columbia University VP&S, New York
Arthur Robin Williams, MD MBE FAPA
Chief Medical Officer
Ophelia Health Inc., New York
Presenter(s)
Non-presenting author(s)
Background & Introduction: Medications for the treatment of opioid use disorder (MOUD) such as buprenorphine are the most effective treatment available for OUD; yet, beyond drug testing results and retention in care, systematically measured clinical outcomes have proven elusive. There is growing interest in integrating systematic monitoring of patient-reported outcomes and measurement-based care as strategies to improve patients' success in treatment.
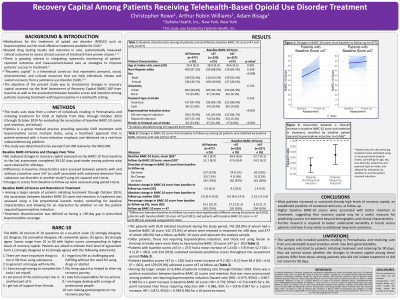
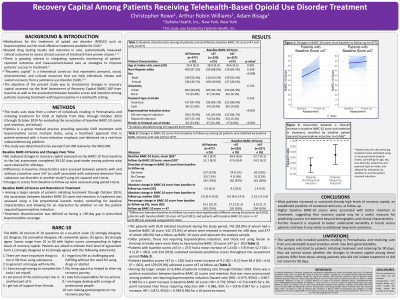
Methods: We analyzed changes in recovery capital assessed via the Brief Assessment of Recovery Capital (BARC-10) from baseline to 30-120 days post-intake among patients with OUD initiating buprenorphine treatment in Pennsylvania from May to October 2023 and who were retained for ≥90 days. Patients initiated and received treatment from Ophelia, a group medical practice providing specialty OUD treatment with buprenorphine across multiple states, using a treatment approach that is patient-centered with a harm-reduction emphasis and delivered via a real-time videoconferencing platform. Differences in baseline characteristics were assessed between patients with and without high "remission-predictive" baseline scores (≥47) using chi-squared and t-tests. Changes in scores from baseline to follow-up were assessed using paired t-tests. Lastly, among a larger sample of patients initiating treatment through October 2024, the association between baseline BARC-10 score and retention in treatment was assessed using a Cox proportional hazards model, controlling for baseline characteristics and allowing for interaction by whether or not the patient required buprenorphine induction.
Results: In all, 791 patients initiated treatment during the study period, 742 (93.8%) of whom had a baseline BARC-10 score, 542 (73.0%) of whom were retained in treatment for ≥90 days, and 477 of whom (88.0%) had a follow-up BARC-10 score and represent the analysis sample. Patients in the analysis sample had a mean age of 39 (SD=9), approximately half (n=236, 49.7%) were female and most were non-Hispanic white (n=409, 87.2%) and paid for their care with insurance (n=417, 87.4%). Older patients, those not requiring buprenorphine induction, and those not using heroin or fentanyl at intake were more likely to have remission-predictive baseline BARC-10 scores (P < .05). Patients with remission-predictive baseline scores (n = 257) had a mean increase of 1.4 (SD = 5.9) from 52.7 (SD = 4.1) (P < .001), and 234 (91%) sustained remission-predictive scores throughout the assessment period. Patients without remission-predictive baseline scores (n = 220) had a mean increase of 9.2 (SD = 8.2) from 38.4 (SD = 6.6) (P < .001), and 129 (59.0%) achieved a remission-predictive score at follow-up. Among the larger sample (n=2,974) used to assess the association between baseline BARC-10 scores and retention, there was a positive association between baseline BARC-10 scores and retention that was more pronounced among patients not requiring buprenorphine induction (hazard ratio [HR] = 0.979, 95%CI = 0.972-0.986 for a 1-point increase in baseline BARC-10 score; HR = 0.807, 95%CI = 0.751-0.866 for a 10-point increase) than those requiring induction (HR = 0.987, 95% CI = 0.978-0.997 for a 1-point increase; HR = 0.880, 95%CI = 0.800-0.955 for a 10-point increase).
Conclusion & Discussion: Most patients had increased or sustained already high levels of recovery capital, an established predictor of sustained remission. Higher baseline BARC-10 scores were associated with better retention in treatment among all patients, with the association more pronounced among patients not requiring induction, suggesting that recovery capital may be a useful measure for predicting success in treatment beyond demographic and clinical characteristics. Further research is required to better understand variability in trends across patients and how it may relate to additional long-term outcomes.
References: Lewis CC, Boyd M, Puspitasari A, et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry. 2019;76(3):324.
Scott K, Lewis CC. Using measurement-based care to enhance any treatment. Cogn Behav Pract. 2015;22(1):49-59.
Marsden J, Tai B, Ali R, Hu L, Rush AJ, Volkow N. Measurement-based care using DSM-5 for opioid use disorder: can we make opioid medication treatment more effective? Addiction. 2019;114(8):1346-1353.
Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, White W. Development and validation of a Brief Assessment of Recovery Capital (BARC-10) for alcohol and drug use disorder. Drug Alcohol Depend. 2017;177:71-76.
Methods: We analyzed changes in recovery capital assessed via the Brief Assessment of Recovery Capital (BARC-10) from baseline to 30-120 days post-intake among patients with OUD initiating buprenorphine treatment in Pennsylvania from May to October 2023 and who were retained for ≥90 days. Patients initiated and received treatment from Ophelia, a group medical practice providing specialty OUD treatment with buprenorphine across multiple states, using a treatment approach that is patient-centered with a harm-reduction emphasis and delivered via a real-time videoconferencing platform. Differences in baseline characteristics were assessed between patients with and without high "remission-predictive" baseline scores (≥47) using chi-squared and t-tests. Changes in scores from baseline to follow-up were assessed using paired t-tests. Lastly, among a larger sample of patients initiating treatment through October 2024, the association between baseline BARC-10 score and retention in treatment was assessed using a Cox proportional hazards model, controlling for baseline characteristics and allowing for interaction by whether or not the patient required buprenorphine induction.
Results: In all, 791 patients initiated treatment during the study period, 742 (93.8%) of whom had a baseline BARC-10 score, 542 (73.0%) of whom were retained in treatment for ≥90 days, and 477 of whom (88.0%) had a follow-up BARC-10 score and represent the analysis sample. Patients in the analysis sample had a mean age of 39 (SD=9), approximately half (n=236, 49.7%) were female and most were non-Hispanic white (n=409, 87.2%) and paid for their care with insurance (n=417, 87.4%). Older patients, those not requiring buprenorphine induction, and those not using heroin or fentanyl at intake were more likely to have remission-predictive baseline BARC-10 scores (P < .05). Patients with remission-predictive baseline scores (n = 257) had a mean increase of 1.4 (SD = 5.9) from 52.7 (SD = 4.1) (P < .001), and 234 (91%) sustained remission-predictive scores throughout the assessment period. Patients without remission-predictive baseline scores (n = 220) had a mean increase of 9.2 (SD = 8.2) from 38.4 (SD = 6.6) (P < .001), and 129 (59.0%) achieved a remission-predictive score at follow-up. Among the larger sample (n=2,974) used to assess the association between baseline BARC-10 scores and retention, there was a positive association between baseline BARC-10 scores and retention that was more pronounced among patients not requiring buprenorphine induction (hazard ratio [HR] = 0.979, 95%CI = 0.972-0.986 for a 1-point increase in baseline BARC-10 score; HR = 0.807, 95%CI = 0.751-0.866 for a 10-point increase) than those requiring induction (HR = 0.987, 95% CI = 0.978-0.997 for a 1-point increase; HR = 0.880, 95%CI = 0.800-0.955 for a 10-point increase).
Conclusion & Discussion: Most patients had increased or sustained already high levels of recovery capital, an established predictor of sustained remission. Higher baseline BARC-10 scores were associated with better retention in treatment among all patients, with the association more pronounced among patients not requiring induction, suggesting that recovery capital may be a useful measure for predicting success in treatment beyond demographic and clinical characteristics. Further research is required to better understand variability in trends across patients and how it may relate to additional long-term outcomes.
References: Lewis CC, Boyd M, Puspitasari A, et al. Implementing measurement-based care in behavioral health: a review. JAMA Psychiatry. 2019;76(3):324.
Scott K, Lewis CC. Using measurement-based care to enhance any treatment. Cogn Behav Pract. 2015;22(1):49-59.
Marsden J, Tai B, Ali R, Hu L, Rush AJ, Volkow N. Measurement-based care using DSM-5 for opioid use disorder: can we make opioid medication treatment more effective? Addiction. 2019;114(8):1346-1353.
Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, White W. Development and validation of a Brief Assessment of Recovery Capital (BARC-10) for alcohol and drug use disorder. Drug Alcohol Depend. 2017;177:71-76.
Learning Objectives:
- Describe the distribution of baseline recovery capital as assessed via the BARC-10 among this sample and how it varies across patient subgroups (e.g. older patients, those requiring induction).
- Describe the average trajectories in recovery capital as assessed via the BARC-10 among patients initiating treatment with higher and lower levels of recovery capital.
- Describe the association between baseline recovery capital as assessed via the BARC-10 and retention in treatment among patients requiring buprenorphine induction and those not requiring buprenorphine induction.
