Back
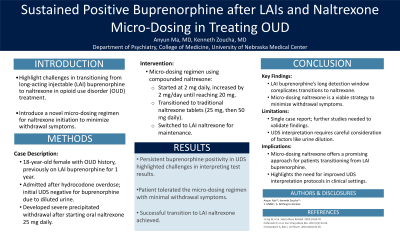
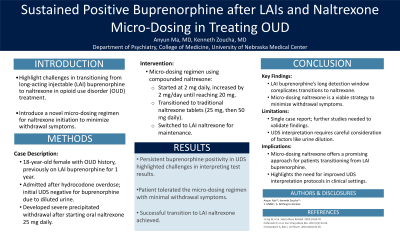
(67) Sustained Positive Buprenorphine after LAIs and Naltrexone Micro-Dosing in Treating OUD
Friday, April 25, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2

Anyun Ma, MD
addiction medicine fellow
University of Nebraska Medical Center, Nebraska
Kenneth Zoucha, MD, FASAM
Associate Professor Psychiatry/Addiction Medicine Division Director
University of Nebraska Medical Center, Nebraska
Presenter(s)
Non-presenting author(s)
Background & Introduction: Oral buprenorphine-naloxone was approved for opioid use disorder (OUD) treatment in 2002 for patients over 16 years of age. A long-acting injectable (LAI) form of buprenorphine was approved in November 2017, allowing patients to receive a monthly subcutaneous injection using the Atrigel Delivery System for slow release. LAI buprenorphine can remain detectable in blood and urine for 6-12 months, which can present unique challenges if a patient’s goal is to transition from an opioid agonist medication to an antagonist medication such as naltrexone.
Case Description: An 18-year-old female with a history of OUD was weaned off LAI buprenorphine after two years of remission, during which she had been receiving LAI buprenorphine for the last year. Six months later, she was admitted following a hydrocodone overdose. She was resuscitated with fluids and initially tested negative for buprenorphine on a urine drug screen (UDS). Nine days later, she was started on oral Naltrexone at 25 mg daily and developed severe precipitated withdrawal symptoms. A repeat UDS was obtained, which was positive for buprenorphine. Despite denying new use of buprenorphine, her UDS remained persistently positive for buprenorphine and its metabolites. Further investigation revealed that the initial urine sample had a specific gravity < 1.010, likely due to urine dilution from fluid resuscitation. A novel treatment regimen, considering a micro-induction method for Naltrexone, was trialed using compounded Naltrexone at 1mg/1ml, starting at 2 mg daily and increasing by 2 mg each day until reaching 20 mg. Subsequently, she transitioned to traditional Naltrexone tablets, initially at 25 mg, and then increasing to 50 mg daily. The patient tolerated this micro-dosing regimen well, experiencing only minimal withdrawal symptoms. Ultimately, oral Naltrexone was switched to LAI Naltrexone.
Conclusion & Discussion: This case highlights the challenges of managing OUD with buprenorphine, particularly LAI forms that can remain in the system for up to 12 months. It also emphasizes the complexity of interpreting UDS results, as aggressive fluid resuscitation can dilute urine, leading to false negatives. In situations where Naltrexone needs to be initiated, this case introduces a novel micro-dosing regimen of compounded Naltrexone, which allowed the patient to tolerate the medication with minimal withdrawal symptoms.
References: 1. Ling W, Shoptaw S, Goodman-Meza D. Depot Buprenorphine Injection In The Management Of Opioid Use Disorder: From Development To Implementation. Subst Abuse Rehabil. 2019 Nov 29;10:69-78. doi: 10.2147/SAR.S155843. Erratum in: Subst Abuse Rehabil. 2020 Jan 31;11:19-20. doi: 10.2147/SAR.S247083. PMID: 31819701; PMCID: PMC6889966.
2. Mannelli P, Peindl KS, Lee T, Bhatia KS, Wu LT. Buprenorphine-mediated transition from opioid agonist to antagonist treatment: state of the art and new perspectives. Curr Drug Abuse Rev. 2012 Mar;5(1):52-63. doi: 10.2174/1874473711205010052. PMID: 22280332; PMCID: PMC3496559.
3. Schwebach A, Ball J. Urine Drug Screening: Minimizing False-Positives and False-Negatives to Optimize Patient Care. US Pharm. 2016;41(8):26-30.
Case Description: An 18-year-old female with a history of OUD was weaned off LAI buprenorphine after two years of remission, during which she had been receiving LAI buprenorphine for the last year. Six months later, she was admitted following a hydrocodone overdose. She was resuscitated with fluids and initially tested negative for buprenorphine on a urine drug screen (UDS). Nine days later, she was started on oral Naltrexone at 25 mg daily and developed severe precipitated withdrawal symptoms. A repeat UDS was obtained, which was positive for buprenorphine. Despite denying new use of buprenorphine, her UDS remained persistently positive for buprenorphine and its metabolites. Further investigation revealed that the initial urine sample had a specific gravity < 1.010, likely due to urine dilution from fluid resuscitation. A novel treatment regimen, considering a micro-induction method for Naltrexone, was trialed using compounded Naltrexone at 1mg/1ml, starting at 2 mg daily and increasing by 2 mg each day until reaching 20 mg. Subsequently, she transitioned to traditional Naltrexone tablets, initially at 25 mg, and then increasing to 50 mg daily. The patient tolerated this micro-dosing regimen well, experiencing only minimal withdrawal symptoms. Ultimately, oral Naltrexone was switched to LAI Naltrexone.
Conclusion & Discussion: This case highlights the challenges of managing OUD with buprenorphine, particularly LAI forms that can remain in the system for up to 12 months. It also emphasizes the complexity of interpreting UDS results, as aggressive fluid resuscitation can dilute urine, leading to false negatives. In situations where Naltrexone needs to be initiated, this case introduces a novel micro-dosing regimen of compounded Naltrexone, which allowed the patient to tolerate the medication with minimal withdrawal symptoms.
References: 1. Ling W, Shoptaw S, Goodman-Meza D. Depot Buprenorphine Injection In The Management Of Opioid Use Disorder: From Development To Implementation. Subst Abuse Rehabil. 2019 Nov 29;10:69-78. doi: 10.2147/SAR.S155843. Erratum in: Subst Abuse Rehabil. 2020 Jan 31;11:19-20. doi: 10.2147/SAR.S247083. PMID: 31819701; PMCID: PMC6889966.
2. Mannelli P, Peindl KS, Lee T, Bhatia KS, Wu LT. Buprenorphine-mediated transition from opioid agonist to antagonist treatment: state of the art and new perspectives. Curr Drug Abuse Rev. 2012 Mar;5(1):52-63. doi: 10.2174/1874473711205010052. PMID: 22280332; PMCID: PMC3496559.
3. Schwebach A, Ball J. Urine Drug Screening: Minimizing False-Positives and False-Negatives to Optimize Patient Care. US Pharm. 2016;41(8):26-30.
Learning Objectives:
- Upon completion, participants will be able to describe key features in clinical applications of long-acting injectable buprenorphine for opioid use disorder (OUD) treatment.
- Upon completion, participants will be able to recognize scenarios, such as fluid resuscitation, that may lead to false negative urine drug screen (UDS) results.
- Upon completion, participant will be able to identify the challenges associated with transitioning patients from agonist to antagonist therapies, and conduct Naltrexone micro-dosing in the transition process.
