Back
(65) Kratom and Kava Use Disorder & Withdrawal Management: A Case Study
Friday, April 25, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2

Cynthia Pathmathasan, MD, MA
Addiction Medicine Fellow Physician
University of Pittsburgh Medical Center, Pennsylvania- JK
Julie A. Kmiec, DO
Associate Professor of Psychiatry
University of PIttsburgh/Department of Psychiatry, Pennsylvania
Presenter(s)
Non-presenting author(s)
Background & Introduction: Kratom, a Southeast Asian herb, and kava, a South Pacific shrub, have surged in popularity in the United States as alternative remedies for pain, fatigue, anxiety, substance use disorder, and withdrawal management. The primary active alkaloid in kratom, 7-hydroxymitragynine interacts with alpha-2 adrenergic and mu-opioid receptors, which can produce stimulant effects at lower doses and sedative effects at higher doses. In contrast, the many kavalactones that make up kava are thought to potentiate GABA-A receptor activity, leading to significant anxiolytic and sedative effects. The unregulated nature and widespread availability of these substances raise concerns about their potential for dependence, development of use disorders, and withdrawal symptoms upon cessation. This case delves into the pharmacological mechanisms of kratom and kava, emphasizing their effects on alpha-2 adrenergic, mu-opioid, and GABA-A receptors. It also examines the symptoms of dependence and withdrawal, quantifying withdrawal severity using the Clinical Opiate Withdrawal Scale (COWS) and the Clinical Institute Withdrawal Assessment (CIWA). Lastly, it presents a comprehensive approach to managing kratom and kava withdrawal, combining targeted pharmacological interventions with ongoing patient support and aftercare.
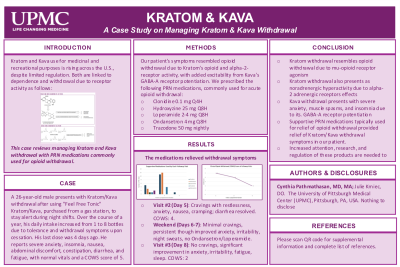
Case Description: We present the case of a 26-year-old man with no significant medical or substance use history who presented to our ambulatory detoxification center with concern for kratom and kava withdrawal. Approximately one year prior, he encountered "Feel Free Classic Tonic," a beverage marketed as combining kratom for energy and kava for relaxation. Initially, he consumed a bottle nightly, which provided focus and energy throughout his night shifts as a law enforcement officer. However, within four weeks, his intake escalated to eight bottles daily as he developed tolerance, transitioning from enhanced energy to significant fatigue, heightened anxiety, and severe abdominal cramping. Encouraged by his family and employer, the patient decided to discontinue the drink. Within 30 minutes of cessation, he experienced nausea and abdominal cramping. Within 72 hours, these symptoms progressed to vomiting, constipation, hot flashes, chills, insomnia, profound fatigue, and debilitating anxiety. The worsening of these symptoms, alongside intense cravings for the beverage, compelled him to seek assistance at our ambulatory detoxification center on Day 4 of withdrawal.
Upon presentation, he reported worsening of existing symptoms with the addition of diarrhea. His vital signs were stable, and a physical examination revealed no significant findings. He scored a five on the Clinical Opiate Withdrawal Scale (COWS) and a seven on the Clinical Institute Withdrawal Assessment (CIWA) scale. His symptoms of restlessness, irritability, nausea, vomiting, diarrhea, hot flashes, chills, and insomnia were attributed to kratom's activity on mu-opioid receptors, while the extreme fatigue and disproportionate anxiety were linked to kava's effects on GABA-A receptors. Given the patient's desire for symptomatic relief, a treatment plan was developed, including as needed clonidine, hydroxyzine, trazodone, loperamide, and ondansetron. Clonidine was selected for its alpha-2 agonism as used in opioid withdrawal to mitigate adrenergic hyperactivity, thereby alleviating symptoms of restlessness and irritability. Hydroxyzine was prescribed to manage anxiety, trazodone for insomnia, loperamide for diarrhea, and ondansetron for nausea and vomiting. The patient attended follow-up appointments on Days 5 and 8, during which he reported significant improvement in his symptoms upon supplementation with these medications, supported by downtrending COWS and CIWA scores. He expressed considerable relief and noted a decrease in anxiety, irritability, and insomnia, along with the complete resolution of nausea, vomiting, diarrhea, and cravings for the beverage. Subsequently, he was successfully referred to our dual diagnosis clinic for ongoing support and aftercare, ensuring a comprehensive approach to managing his recovery.
Conclusion & Discussion: This case highlights the complexities of managing withdrawal from substances like kratom and kava, which, while increasingly accessible, remain largely unregulated in the United States. It emphasizes the need for healthcare professionals to understand the pharmacological mechanisms of these substances, recognize withdrawal symptoms, and implement targeted pharmacological interventions for effective relief. In this case, the use of clonidine, hydroxyzine, trazodone, loperamide, and ondansetron alleviated immediate symptoms and supported the patient’s transition to ongoing care, demonstrating the importance of integrated approaches in substance use recovery. The case also stresses the urgent need for greater awareness, research, and regulation of kratom and kava to protect public health. However, there are notable limitations, including a lack of long-term follow-up data, which restricts understanding of the sustained effectiveness of the treatment. The small sample size and variability in individual responses further limit the generalizability of the findings. Additionally, the patient had a strong support system, paid time off, reliable transportation, and access to technology, all of which facilitated his ability to seek and sustain treatment. These advantages, however, are atypical for many individuals with substance use disorders and highlight the need for more equitable access to resources in the broader population.
References: Eastlack, S. C., Cornett, E. M., & Kaye, A. D. (2020). Kratom—Pharmacology, clinical implications, and outlook: A comprehensive review. Pain Therapy, 9(1), 55-69. https://doi.org/10.1007/s40122-020-00151-x
Galbis-Reig, D. (2016). A case report of kratom addiction and withdrawal. WMJ. Retrieved from https://wmjonline.org
Hill, K., Grundmann, O., Smith, K. E., & Stanciu, C. N. (2024). Prevalence of kratom use disorder among kratom consumers. Journal of Addiction Medicine, 18(3), 306-312. https://doi.org/10.1097/ADM.0000000000001290
Sarris, J., LaPorte, E., & Schweitzer, I. (2011). Kava: A comprehensive review of efficacy, safety, and psychopharmacology. Australian & New Zealand Journal of Psychiatry, 45(1), 27-35. https://doi.org/10.3109/00048674.2010.522554
Veltri, C., & Grundmann, O. (2019). Current perspectives on the impact of kratom use. Substance Abuse: Research and Treatment, 10, 23-31. https://doi.org/10.2147/SAR.S164261
Case Description: We present the case of a 26-year-old man with no significant medical or substance use history who presented to our ambulatory detoxification center with concern for kratom and kava withdrawal. Approximately one year prior, he encountered "Feel Free Classic Tonic," a beverage marketed as combining kratom for energy and kava for relaxation. Initially, he consumed a bottle nightly, which provided focus and energy throughout his night shifts as a law enforcement officer. However, within four weeks, his intake escalated to eight bottles daily as he developed tolerance, transitioning from enhanced energy to significant fatigue, heightened anxiety, and severe abdominal cramping. Encouraged by his family and employer, the patient decided to discontinue the drink. Within 30 minutes of cessation, he experienced nausea and abdominal cramping. Within 72 hours, these symptoms progressed to vomiting, constipation, hot flashes, chills, insomnia, profound fatigue, and debilitating anxiety. The worsening of these symptoms, alongside intense cravings for the beverage, compelled him to seek assistance at our ambulatory detoxification center on Day 4 of withdrawal.
Upon presentation, he reported worsening of existing symptoms with the addition of diarrhea. His vital signs were stable, and a physical examination revealed no significant findings. He scored a five on the Clinical Opiate Withdrawal Scale (COWS) and a seven on the Clinical Institute Withdrawal Assessment (CIWA) scale. His symptoms of restlessness, irritability, nausea, vomiting, diarrhea, hot flashes, chills, and insomnia were attributed to kratom's activity on mu-opioid receptors, while the extreme fatigue and disproportionate anxiety were linked to kava's effects on GABA-A receptors. Given the patient's desire for symptomatic relief, a treatment plan was developed, including as needed clonidine, hydroxyzine, trazodone, loperamide, and ondansetron. Clonidine was selected for its alpha-2 agonism as used in opioid withdrawal to mitigate adrenergic hyperactivity, thereby alleviating symptoms of restlessness and irritability. Hydroxyzine was prescribed to manage anxiety, trazodone for insomnia, loperamide for diarrhea, and ondansetron for nausea and vomiting. The patient attended follow-up appointments on Days 5 and 8, during which he reported significant improvement in his symptoms upon supplementation with these medications, supported by downtrending COWS and CIWA scores. He expressed considerable relief and noted a decrease in anxiety, irritability, and insomnia, along with the complete resolution of nausea, vomiting, diarrhea, and cravings for the beverage. Subsequently, he was successfully referred to our dual diagnosis clinic for ongoing support and aftercare, ensuring a comprehensive approach to managing his recovery.
Conclusion & Discussion: This case highlights the complexities of managing withdrawal from substances like kratom and kava, which, while increasingly accessible, remain largely unregulated in the United States. It emphasizes the need for healthcare professionals to understand the pharmacological mechanisms of these substances, recognize withdrawal symptoms, and implement targeted pharmacological interventions for effective relief. In this case, the use of clonidine, hydroxyzine, trazodone, loperamide, and ondansetron alleviated immediate symptoms and supported the patient’s transition to ongoing care, demonstrating the importance of integrated approaches in substance use recovery. The case also stresses the urgent need for greater awareness, research, and regulation of kratom and kava to protect public health. However, there are notable limitations, including a lack of long-term follow-up data, which restricts understanding of the sustained effectiveness of the treatment. The small sample size and variability in individual responses further limit the generalizability of the findings. Additionally, the patient had a strong support system, paid time off, reliable transportation, and access to technology, all of which facilitated his ability to seek and sustain treatment. These advantages, however, are atypical for many individuals with substance use disorders and highlight the need for more equitable access to resources in the broader population.
References: Eastlack, S. C., Cornett, E. M., & Kaye, A. D. (2020). Kratom—Pharmacology, clinical implications, and outlook: A comprehensive review. Pain Therapy, 9(1), 55-69. https://doi.org/10.1007/s40122-020-00151-x
Galbis-Reig, D. (2016). A case report of kratom addiction and withdrawal. WMJ. Retrieved from https://wmjonline.org
Hill, K., Grundmann, O., Smith, K. E., & Stanciu, C. N. (2024). Prevalence of kratom use disorder among kratom consumers. Journal of Addiction Medicine, 18(3), 306-312. https://doi.org/10.1097/ADM.0000000000001290
Sarris, J., LaPorte, E., & Schweitzer, I. (2011). Kava: A comprehensive review of efficacy, safety, and psychopharmacology. Australian & New Zealand Journal of Psychiatry, 45(1), 27-35. https://doi.org/10.3109/00048674.2010.522554
Veltri, C., & Grundmann, O. (2019). Current perspectives on the impact of kratom use. Substance Abuse: Research and Treatment, 10, 23-31. https://doi.org/10.2147/SAR.S164261
Learning Objectives:
- Upon completion, participants will be able to describe the pharmacological mechanisms of action for kratom and kava, including their effects on alpha-2 adrenergic, mu-opioid, and GABA-A receptors.
- Upon completion, participants will be able to list kratom and kava withdrawal symptoms and track them via Clinical Opiate Withdrawal Scale (COWS) and Clinical Institute Withdrawal Assessment (CIWA).
- Upon completion, participants will be able to develop a comprehensive treatment for kratom and kava withdrawal, combining supportive pharmacological interventions, ongoing patient support, and aftercare.
