Back
(126) Buprenorphine Rescue for XR Naltrexone-Precipitated Opioid Withdrawal: A Case Report
Saturday, April 26, 2025
9:45 AM – 1:15 PM
Location: Aurora Ballroom Pre-Function, Level 2

Hannah Kissel-Smith, MD
Addiction Medicine Fellow
VCU Health, Virginia
Megan Lemay, MD
Associate Professor
Virginia Commonwealth University, Virginia
Presenter(s)
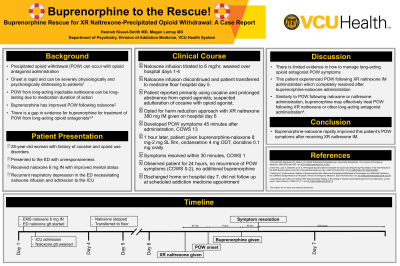
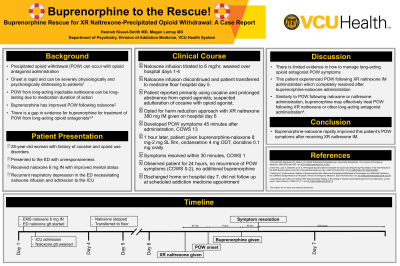
Background & Introduction: Precipitated opioid withdrawal (POW) is a known complication of opioid antagonist administration in the setting of opioid agonist use. Compared to opioid withdrawal related to abstinence from opioid agonists, symptoms of POW are rapid in onset and typically more severe, which can be severely psychologically and physiologically stressful for patients(1). The risk of POW for opioid use disorder is further magnified in the setting of long-acting injectable naltrexone administration due to the duration of medication effect. There is no consensus on opioid antagonist-induced POW treatment, though strategies have typically focused on supportive care and symptom mitigation rather than activation of the mu-opioid receptors(1). Several studies have reported using the partial opioid agonist buprenorphine with significant improvement in POW following naloxone administration(2,3), though its utility following longer acting opioid antagonists such as naltrexone and nalmefene is less well described(3,4). We present a case of POW following injectable XR naltrexone administration that rapidly improved with buprenorphine.
Case Description: A 28-year-old female with a history of cocaine and opioid use disorder presented to the emergency department for unresponsiveness after a suspected opioid overdose. Prior to arrival at the emergency department, the patient received naloxone 6 mg intranasally with improved level of consciousness. Due to ongoing respiratory depression, the patient was started on a naloxone infusion was admitted to the ICU for further management. The naloxone infusion was titrated to a maximum of 6 mg/hr and was slowly weaned over hospital days 1 through 4. Clinical Opiate Withdrawal Scale scores documented throughout naloxone infusion ranged from 1 to 7. After discontinuation of the naloxone infusion on hospital day 5, the patient was transferred to the medicine floor for further management. The patient endorsed cocaine use but had not intentionally used opioids in several years. She expressed a treatment goal of harm reduction given concern for adulteration of cocaine with an opioid agonist. She received XR naltrexone 380 mg intramuscular injection on hospital day 6. Within 45 minutes of administration of XR naltrexone administration the patient developed signs and symptoms of POW with a Clinical Opiate Withdrawal Scale (COWS) score of 13. Symptoms included nausea, vomiting, hot flashes, chills, and severe restlessness. She received buprenorphine-naloxone 8 mg-2 mg sublingual film, ondansetron 4 mg orally, and clonidine 0.1 mg orally approximately 1 hour after XR naltrexone administration. Her symptoms resolved within 30 minutes after administration of buprenorphine with COWS of 1 (heart rate of 81). The patient was observed for 24 hours following buprenorphine administration and did not have recurrence of significant symptoms (COWS 0-2), nor did she require further medications for POW-related symptoms. She was discharged home on hospital day 7 without symptoms of opioid withdrawal. The patient had an appointment with the addiction medicine clinic at the time of discharge but did not present to the clinic.
Conclusion & Discussion: In this case we describe a patient admitted for opioid overdose requiring naloxone infusion who experienced POW after XR naltrexone administration with complete resolutions of symptoms after a single dose of buprenorphine-naloxone 8 mg-2 mg sublingual film. While POW is a known potential outcome following administration of an opioid antagonist, there is limited evidence on best management strategies to mitigate these very distressing symptoms. Buprenorphine is known to reduce symptoms of POW from partial opioid agonist and short-acting opioid antagonist administration, but this case suggests that there may additionally be a role of buprenorphine for treatment of long-acting opioid antagonist-induced POW. Several cases have reported rapid improvement of naltrexone-induced POW with buprenorphine ranging from 8 to 22 mg(1), though to our knowledge there have been no reports of buprenorphine used for treatment of POW from XR injectable naltrexone. In this case, XR injectable naltrexone was not expected to cause POW, as this patient did not have significant withdrawal symptoms in the preceding 5 days while on a naloxone infusion. Interestingly, this patient did not require further buprenorphine administration prior to discharge and did not have recurrence of POW symptoms.
References: 1. Kunzler NM, Wightman RS, Nelson LS. Opioid Withdrawal Precipitated by Long-Acting Antagonists. The Journal of Emergency Medicine. 2020;58(2):245-253. doi:10.1016/j.jemermed.2019.12.015
2. Hern HG, Lara V, Goldstein D, et al. Prehospital Buprenorphine Treatment for Opioid Use Disorder by Paramedics: First Year Results of the EMS Buprenorphine Use Pilot. Prehospital Emergency Care. 2023;27(3):334-342. doi:10.1080/10903127.2022.2061661
3. Herring AA. Postoverdose Initiation of Buprenorphine After Naloxone-Precipitated Withdrawal Is Encouraged as a Standard Practice in the California Bridge Network of Hospitals. Annals of Emergency Medicine. 2020;75(4):552-553. doi:10.1016/j.annemergmed.2019.12.015
4. Szczesniak LM, Calleo VJ, Sullivan RW. Buprenorphine therapy in the setting of induced opioid withdrawal from oral naltrexone: a case report. Harm Reduct J. 2020;17(1):71. doi:10.1186/s12954-020-00417-9
Case Description: A 28-year-old female with a history of cocaine and opioid use disorder presented to the emergency department for unresponsiveness after a suspected opioid overdose. Prior to arrival at the emergency department, the patient received naloxone 6 mg intranasally with improved level of consciousness. Due to ongoing respiratory depression, the patient was started on a naloxone infusion was admitted to the ICU for further management. The naloxone infusion was titrated to a maximum of 6 mg/hr and was slowly weaned over hospital days 1 through 4. Clinical Opiate Withdrawal Scale scores documented throughout naloxone infusion ranged from 1 to 7. After discontinuation of the naloxone infusion on hospital day 5, the patient was transferred to the medicine floor for further management. The patient endorsed cocaine use but had not intentionally used opioids in several years. She expressed a treatment goal of harm reduction given concern for adulteration of cocaine with an opioid agonist. She received XR naltrexone 380 mg intramuscular injection on hospital day 6. Within 45 minutes of administration of XR naltrexone administration the patient developed signs and symptoms of POW with a Clinical Opiate Withdrawal Scale (COWS) score of 13. Symptoms included nausea, vomiting, hot flashes, chills, and severe restlessness. She received buprenorphine-naloxone 8 mg-2 mg sublingual film, ondansetron 4 mg orally, and clonidine 0.1 mg orally approximately 1 hour after XR naltrexone administration. Her symptoms resolved within 30 minutes after administration of buprenorphine with COWS of 1 (heart rate of 81). The patient was observed for 24 hours following buprenorphine administration and did not have recurrence of significant symptoms (COWS 0-2), nor did she require further medications for POW-related symptoms. She was discharged home on hospital day 7 without symptoms of opioid withdrawal. The patient had an appointment with the addiction medicine clinic at the time of discharge but did not present to the clinic.
Conclusion & Discussion: In this case we describe a patient admitted for opioid overdose requiring naloxone infusion who experienced POW after XR naltrexone administration with complete resolutions of symptoms after a single dose of buprenorphine-naloxone 8 mg-2 mg sublingual film. While POW is a known potential outcome following administration of an opioid antagonist, there is limited evidence on best management strategies to mitigate these very distressing symptoms. Buprenorphine is known to reduce symptoms of POW from partial opioid agonist and short-acting opioid antagonist administration, but this case suggests that there may additionally be a role of buprenorphine for treatment of long-acting opioid antagonist-induced POW. Several cases have reported rapid improvement of naltrexone-induced POW with buprenorphine ranging from 8 to 22 mg(1), though to our knowledge there have been no reports of buprenorphine used for treatment of POW from XR injectable naltrexone. In this case, XR injectable naltrexone was not expected to cause POW, as this patient did not have significant withdrawal symptoms in the preceding 5 days while on a naloxone infusion. Interestingly, this patient did not require further buprenorphine administration prior to discharge and did not have recurrence of POW symptoms.
References: 1. Kunzler NM, Wightman RS, Nelson LS. Opioid Withdrawal Precipitated by Long-Acting Antagonists. The Journal of Emergency Medicine. 2020;58(2):245-253. doi:10.1016/j.jemermed.2019.12.015
2. Hern HG, Lara V, Goldstein D, et al. Prehospital Buprenorphine Treatment for Opioid Use Disorder by Paramedics: First Year Results of the EMS Buprenorphine Use Pilot. Prehospital Emergency Care. 2023;27(3):334-342. doi:10.1080/10903127.2022.2061661
3. Herring AA. Postoverdose Initiation of Buprenorphine After Naloxone-Precipitated Withdrawal Is Encouraged as a Standard Practice in the California Bridge Network of Hospitals. Annals of Emergency Medicine. 2020;75(4):552-553. doi:10.1016/j.annemergmed.2019.12.015
4. Szczesniak LM, Calleo VJ, Sullivan RW. Buprenorphine therapy in the setting of induced opioid withdrawal from oral naltrexone: a case report. Harm Reduct J. 2020;17(1):71. doi:10.1186/s12954-020-00417-9
Learning Objectives:
- Upon completion, participants will be able to recognize symptoms of precipitated opioid withdrawal following long-acting opioid antagonist administration.
- Upon completion, participants will be able to describe buprenorphine as a potential treatment for precipitated opioid withdrawal from XR naltrexone administration.
- Upon completion, participants will be able to demonstrate understanding of potential for precipitated opioid withdrawal caused by long-acting opioid antagonists.
